Heart:新冠肺炎患者心脏代谢性并发症及种族对心血管/肾脏并发症的影响
2022-01-22 从医路漫漫 MedSci原创
截至2021年4月,SARS-CoV-2在全球已感染超过1.4亿人,夺走300多万人的生命。感染后,病程(新冠肺炎)各不相同,从无症状的轻症感染到出现严重的并发症和死亡。
背景:截至2021年4月,SARS-CoV-2在全球已感染超过1.4亿人,夺走300多万人的生命。感染后,病程(新冠肺炎)各不相同,从无症状的轻症感染到出现严重的并发症和死亡。需要住院的人预后更差,在美国和英国的死亡风险为10%-26%。
非白种人或患有多种慢性疾病的人群发现更易患严重的COVID-19疾病、住院心血管并发症和死亡,特别是心脏代谢健康受损已成为严重COVID-19疾病加速的重要因素。超过25%的COVID-19住院患者患有心脏代谢疾病,包括高血压、肥胖、糖尿病和慢性心脏病这些并发症是导致COVID-19结果恶化的主要慢性疾病。除了与心脏代谢状况相关的基线风险外,最近的研究表明,COVID-19可导致急性心血管损伤,包括心律失常、心脏骤停、心肌梗死和心力衰竭。这些损害反过来会导致慢性心血管损伤或死亡,甚至对那些没有心血管疾病的人也是如此。COVID-19与心血管并发症相关的可能机制包括细胞因子的释放(“细胞因子风暴”)、肾素-血管紧张素-醛固酮系统和凝血系统的失调,以及急性感染期的斑块破裂
目的:利用全国新冠肺炎住院患者的大型数据库,调查心脏代谢状况、并发症和种族对住院心血管并发症和死亡风险的影响。
由于COVID-19患者往往结合了不同的高风险特征,很难知道哪些是最重要的,也很难知道非白种人中COVID-19并发症的部分或全部高风险是否可以用他们的心脏代谢条件来解释。为了揭示导致COVID-19不良预后的各种因素的相对重要性,需要大量、表型良好的样本,并覆盖这些因素。因此,本研究在COVID-19住院患者的一个具有全国代表性的大样本中,调查了多种心脏代谢疾病和患者种族对心血管/肾脏并发症和死亡风险的贡献。
方法:对2020年2月6日至2021年3月16日期间因新冠肺炎住院的302家英国医疗机构进行了一项多中心前瞻性队列研究。采用Logistic模型探讨基线患者种族、心脏代谢状况和并发症(0、1、2、>2种情况)与住院心血管并发症(心力衰竭、心律失常、心脏缺血、心脏骤停、凝血并发症、中风)、肾损伤和死亡之间的关系。
结果:65624例新冠肺炎患者中,44598例(68.0%)入院时至少有一种心脏代谢异常。24609例(38.0%)患者发生心血管/肾脏并发症或死亡。基线心脏代谢状况与住院并发症的发生几率增加独立相关,当存在心脏代谢多发病时,这种风险也会增加。例如,与无心脏代谢性疾病相比,1、2或≥3状态分别与心血管/肾脏并发症的风险增加1.46(95%CI 1.39~1.5 4)、2.0 4(95%CI 1.93~2.15)和3.10(95%CI 2.92~3.2 9)倍。在全死因死亡中也观察到了类似的模式。与白人相比,南亚(OR 1.19,95%CI 1.10~1.29)和黑人(OR 1.53~95%CI 1.37~1.72)民族发生心血管/肾脏并发症的风险较高。
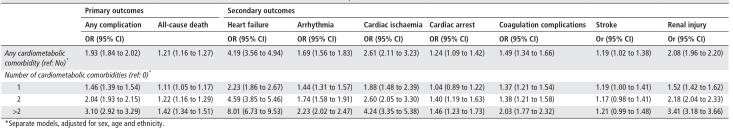
表1 基线心脏代谢合并症、心血管/肾脏并发症和全因死亡之间的关系

图1 基线心脏代谢多发病率与(1)医院内任何心血管/肾脏并发症和(2)全因死亡(经性别、年龄和种族调整后)之间的相关性。

表2 种族、心血管/肾脏并发症与全因死亡之间的关系

图2 (A)基线心脏代谢多病与医院内每一心血管/肾脏并发症之间的关联(根据性别、年龄和种族进行调整)。(B)基线心脏代谢多病与医院内每一心血管/肾脏并发症之间的相关性(根据性别、年龄和种族进行调整)。
结论:在住院的新冠肺炎患者中,心血管并发症或死亡影响略低于所有患者的一半,南亚或黑人以及心脏代谢并发症患者风险最高。
原文出处: Norris T, Razieh C, Zaccardi F,et al.Impact of cardiometabolic multimorbidity and ethnicity on cardiovascular/renal complications in patients with COVID-19.Heart 2021 Dec 15
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#代谢性#
42
#肾脏并发症#
27
#并发#
37
#心脏代谢#
44
#ART#
25
#HEART#
28