2022 ASCO:YAP-1对ES-SCLC患者免疫治疗疗效的预测价值
2022-05-31 紫菀款冬 MedSci原创
探讨Yes相关蛋白1(YAP-1)的表达状态是否可以筛选广泛期小细胞肺癌(ES-SCLC)患者中免疫治疗的优势人群。
背景:IMpower133显示依托泊苷/顺铂卡铂联合阿特珠单抗(ECT)方案对广泛期小细胞肺癌(ES-SCLC)的无进展生存期(PFS)和总生存期(OS)均有益处,但绝对益处有限。以前的研究通过RNA-seq聚类分析对SCLC患者进行分类,以探索治疗的优势人群,但临床应用困难。该研究旨在探讨Yes相关蛋白1(YAP-1)的表达状态是否可以筛选ES-SCLC患者中免疫治疗的优势人群。
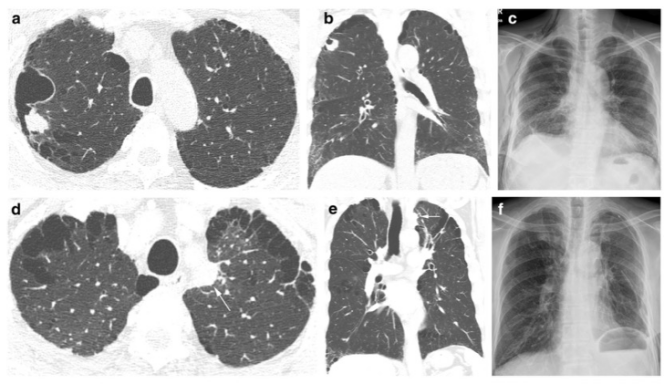
方法:该研究选择了2018年1月至2021年7月在广东省人民医院接受治疗的ES-SCLC患者,共招募21名接受了ECT方案的ES-SCLC患者,获得他们的甲醛固定、石蜡包埋样本。完全缓解(CR)、部分缓解(PR)、疾病稳定(SD)和进展性疾病(PD)的评估依据实体瘤疗效评估标准(RECIST)1.1版。对YAP-1(ET1608-30,1/100)进行免疫组化(IHC)。H评分由IHC Profiler计算。所有统计分析均使用SPSS 22.0、X-tile 3.6.1和Excel进行评估。P<0.05被认为具有统计学意义。
结果:下表提供了基线信息。有应答者(CR/PR患者)和无应答者的H评分中位数分别为13.97(95%CI:8.97-16.30)和23.72(95%CI:8.13-75.40),差异显著(P<0.05)。Spearman的H评分与PFS呈负相关(r=-0.603)。根据H评分的截止值,将患者分为两组,即低表达组(H评分≤25.00,n=16)和高表达组(H评分>25.00,n=5)。这两组患者的PFS中位数分别为7.1m(95%CI:2.6-11.6m)和3.4m(95%CI:0.9-5.9m)。PFS的K-M曲线有显著性差异(P<0.05)。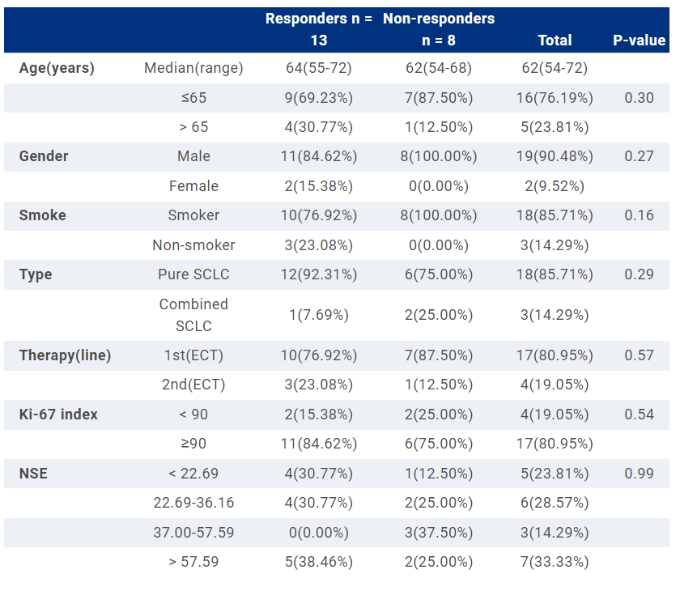
结论:该研究结果初步表明YAP-1蛋白具有潜在的疗效预测价值,ES-SCLC患者YAP-1蛋白表达水平与ECT疗效呈负相关。
原始出处:
Yuqing Chen, Xu-Hui Guan, Ling-Ling Gao, et al. The predictive value of YAP-1 for efficacy of immunotherapy among patients with ES-SCLC.
https://meetings.asco.org/abstracts-presentations/207509
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#YAP#
49
#ASC#
40
#SCLC患者#
64
#预测价值#
44
好东西 谢谢分享
51