时隔六年,又一重大发现发表于《新英格兰杂志》: Sotatercept用于治疗肺动脉高压
2021-09-22 刘少飞 MedSci原创
肺动脉高压(PAH)的特征是肺血管重构,细胞增殖和长期预后不良。BMP信号通路的功能异常与遗传性和特发性PAH相关。
Sotatercept for the Treatment of Pulmonary Arterial Hypertension.
影响因子:74.699
PMID:33789009
期刊年卷:N Engl J Med 2021 Apr 01;384(13)
第一作者:Marc Humbert, M.D

研究背景:
肺动脉高压(PAH)的特征是肺血管重构,细胞增殖和长期预后不良。BMP信号通路的功能异常与遗传性和特发性PAH相关。Sotatercept,一种新型融合蛋白,结合激活素和生长分化因子,可恢复growth-promoting 和 growth-inhibiting 信号通路之间的平衡。
研究方法:
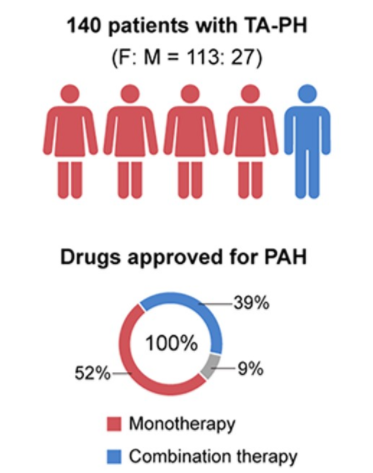
在这项为期24周的多中心试验中,研究随机分配了106位接受肺动脉高压背景治疗的成人接受皮下注射的sotertercept,一组为每3周以0.3毫克/千克的剂量服用,另一组每3周0.7毫克/千克的剂量服用,以及安慰剂组。
主要终点是从基线到第24周肺血管阻力的变化。
三组之间的基线特征相似。
研究结果:
从基线到第24周:
sotatercept 0.3 mg组与安慰剂组之间肺血管阻力的最小二乘均方差为-145.8 dyn·sec··cm(95%置信区间[CI],-241.0至- 50.6;P = 0.003)。
Sotatercept 0.7 mg组与安慰剂组之间的最小二乘均差为-239.5 dyn·ssec·s·cm(95%CI,-329.3至-149.7; P <0.001)。
在第24周时:
Sotatercept 0.3 mg组与安慰剂组之间的基线在6分钟步行距离内的变化的最小二乘均方差为29.4 m(95%CI,3.8至55.0)。
Sotatercept 0.7 mg组与安慰剂组之间的最小二乘均差为21.4 m(95%CI,-2.8至45.7)。
Sotatercept还与N端前B型利钠肽水平降低有关。
血小板减少症和血红蛋白水平升高是最常见的血液学不良事件。
sotatercept 0.7 mg组的一名患者死于心脏骤停。
结论:Sotatercept治疗可降低接受肺动脉高压背景治疗的患者的肺血管阻力。
Editorial from John H. Newman, M.D.
为什么抑制TGF-β途径是一种有效的方法?
答案在于遗传学的发现,大约70%至80%的HPAH和大约20%至30%的IPAH是涉及BMPR2的功能受损的后果.
BMPR2的突变和损伤可能导致其他增生性和促炎性TGF-β途径中的功能增强,可能导致肺血管阻塞和纤维化。
因此,我们推断未突变的BMPR2充当这些疾病的“刹车”。疾病途径和突变的BMPR2不能有效地阻断它们。为什么BMPR2除了参与骨骼功能外,还参与纤维化和小肺小动脉的阻塞仍然是一个谜。
融合蛋白sotatercept的本质是什么?
Sotatercept被设计为结合和捕获TGF-β家族配体激活素。它由与人IgG1 Fc结构域融合的IIA型人类激活素受体的胞外结构域组成。激活素受体参与遗传性出血性毛细血管扩张,其参与肺动脉高压很少见,但众所周知。融合蛋白中的激活素受体与细胞外激活素结合,阻止其激活天然细胞激活素受体,从而将其捕获。Fc区似乎是蛋白质的稳定部分。
Sotatercept是一流的药物,具有极好的理论潜力,可重新平衡TGF-β系统,在24周的试验中,它显示出有益的效果。试验结果证明需要进行更长的试验并纳入更多的患者。还可能需要测试TGF-β大家族中可能与肺动脉高压发展有关的其他配体和受体。在试验过程中观察到的不良反应是可以控制的,并且在很大程度上是可以预测的。鉴于先前的研究结果,在某些患者中血红蛋白水平升高是可以预测的,因为TGF-β参与了造血作用。其他对炎症反应,伤口愈合,骨骼功能和右心室功能的潜在长期影响 必须等待更长的观察。对于这种困难和致命的疾病,这是一个有利的进步。
原文链接:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#重大发现#
49
#新英格兰#
40
#动脉高压#
28
#Sotatercept#
51