Cell Death Dis:新型环状RNA circXPO1促进肺腺癌的发生发展
2020-12-12 MedSci原创 MedSci原创
肺癌是全球范围内肿瘤相关死亡的主要原因之一。肺腺癌(LUAD)作为肺癌的主要组织学类型,在中国,LUAD的发病率逐年增加。尽管目前已开发出了针对LUAD的新的治疗方法,但患者的5年生存率仅为12%至1
肺癌是全球范围内肿瘤相关死亡的主要原因之一。肺腺癌(LUAD)作为肺癌的主要组织学类型,在中国,LUAD的发病率逐年增加。尽管目前已开发出了针对LUAD的新的治疗方法,但患者的5年生存率仅为12%至15%。因此,进一步探索LUAD的分子机制和鉴定相应的生物标记物能够提高患者的治疗效果。
既往研究显示,非编码RNA(ncRNA)在各种类型的癌症中起着至关重要的作用。环状RNA(circRNA)作为一类独特的非编码RNA,在哺乳动物细胞和组织中具有独特的特性和功能。circRNA在多种疾病(包括癌症)中发挥调节作用,并行使众所周知的“ miRNA分子海绵”的功能。
然而,目前关于基因组改变区域的非编码RNA的研究很少,特别是circRNA。该研究前期通过RNA测序发现,在LUAD肿瘤组织中一些circRNA的表达水平上调。
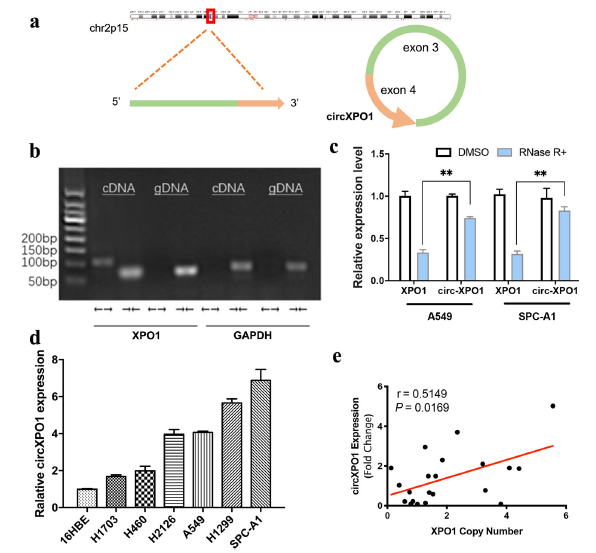
circXPO1的转录本
研究人员在LUAD中发现了一种新的circRNA,circXPO1,其来自于一个公认的癌症治疗靶标XPO1。circXPO1是由XPO1基因的3号外显子和4号外显子反向剪接形成的。相比于相邻的非肿瘤组织,circXPO1在LUAD组织中高表达,而circXPO1的高表达水平与更差的总体生存率相关。
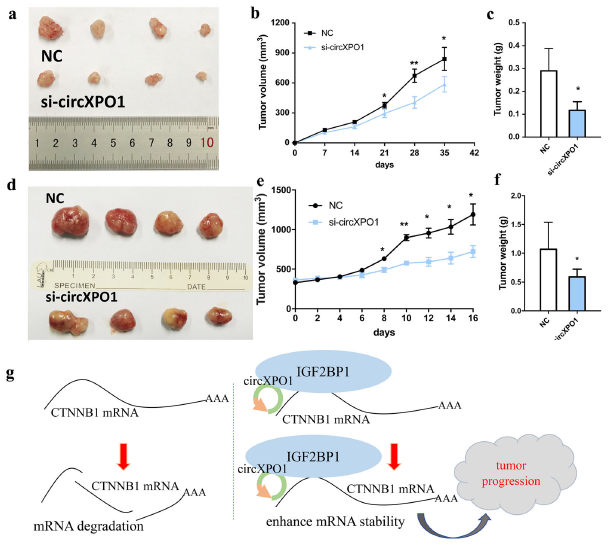
研究人员发现,circXPO1的表达水平与XPO1基因的拷贝数呈正相关。机制研究显示,circXPO1可以与IGF2BP1结合并增强CTNNB1 mRNA的稳定性,并最终促进LUAD的发生发展。在LUAD患者衍生的移植瘤模型中,在肿瘤内注射特异性的靶向circXPO1的胆固醇缀合siRNA能够有效的抑制肿瘤的生长。
circXPO1促进LUAD肿瘤的生长
综上所述,这些结果表明,circXPO1对于LUAD的发生发展至关重要,其可能作为该疾病的不良预后和治疗的生物标志物。
原始出处:
Huang, Q., Guo, H., Wang, S. et al. A novel circular RNA, circXPO1, promotes lung adenocarcinoma progression by interacting with IGF2BP1. Cell Death Dis 11, 1031 (02 December 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Dis#
29
#CEL#
33
#Cell#
24
#发生发展#
31
#Death#
26
肺腺癌(LUAD)作为肺癌的主要组织学类型,在中国,LUAD的发病率逐年增加。尽管目前已开发出了针对LUAD的新的治疗方法,但患者的5年生存率仅为12%至15%。#肺腺癌##环状RNA#
129
学习了
82
学习了
76