JCEM:糖尿病患者收缩压降低与血管结局之间的因果关系
2022-06-18 MedSci原创 MedSci原创
收缩压降低与糖尿病CAD和肾病风险降低之间存在因果关系。这为终身控制收缩压在预防糖尿病相关血管预后方面的有益作用提供了遗传学证据。
糖尿病和高血压已被确认为心血管疾病(CVD)的两大主要危险因素。血糖或血压失控与严重的发病率和死亡率相关,两者并存是动脉粥样硬化性心血管疾病(ASCVD)、心力衰竭和肾脏疾病极强的致病因素。降低收缩压对糖尿病患者临床结局的影响目前存在争议。
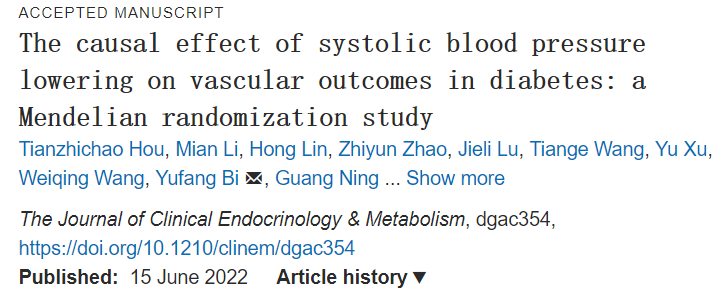
近日,内分泌和代谢性疾病领域权威杂志Journal of Clinical Endocrinology & Metabolism上发表了一篇研究文章,研究人员采用双样本孟德尔随机化(MR)研究收缩压降低对糖尿病患者大血管和微血管预后风险的因果关系。
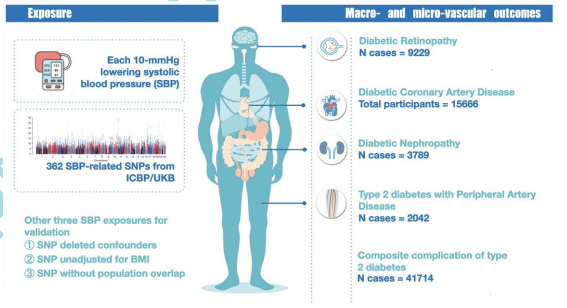
研究人员从一项大型全基因组关联研究(n=299024)和英国生物银行(n=375256)中选取了362个与收缩压相关的遗传变异作为研究对象。研究人员评估了多达60742例糖尿病患者的5个大血管和微血管并发症,包括冠状动脉疾病(CAD)、外周动脉疾病(PAD)、肾病、视网膜病变和复合并发症。所有病例均伴有糖尿病。研究人员进行了7项敏感性分析,并将目前的MR结果与普通人群和临床试验的结果进行了比较,且进行了随访分析。
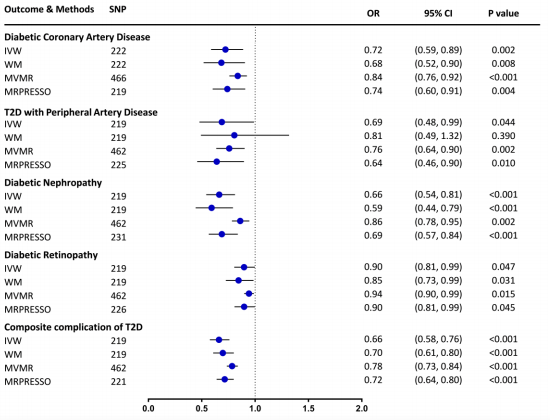
收缩压每降低10mmHg,遗传易感性与28%的冠心病风险降低显著相关(比值比[OR]为0.72,95%置信区间[CI]为0.59-0.89,p=0.002),34%的肾病风险降低(OR为0.66,95%CI为0.54-0.81,p<0.001),34%的复合并发症风险降低(OR为0.66,95%CI为0.58-0.76,p<0.001);而收缩压与PAD(OR为0.69,95%CI为0.48-0.99)和视网膜病变(OR为0.90,95%CI为0.81-0.99)风险降低相关。糖尿病的MR结果与普通人群和临床试验的结果相似。
由此可见,收缩压降低与糖尿病CAD和肾病风险降低之间存在因果关系。这为终身控制收缩压在预防糖尿病相关血管预后方面的有益作用提供了遗传学证据。
原始出处:
Tianzhichao Hou,et al.The causal effect of systolic blood pressure lowering on vascular outcomes in diabetes: a Mendelian randomization study.JCEM.2022.https://academic.oup.com/jcem/advance-article-abstract/doi/10.1210/clinem/dgac291/6590071?redirectedFrom=fulltext
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#收缩压#
44
#JCEM#
42
#JCE#
0
#糖尿病患者#
42
不错,学习了。
47