Cancers:EGFR/ALK阴性晚期NSCLC患者在免疫治疗获批一线治疗后的生存获益:来自真实世界研究数据
2021-09-28 yd2015 MedSci原创
研究表明,免疫检查点抑制剂(ICI)的获批明显改善EGFR/ALK阴性晚期NSCLC患者的OS。PS≥1, 骨转移和肝转移是不良预后因素。
在非小细胞肺癌(NSCLC)患者中选择合适的患者进行免疫检查点抑制剂(ICI)治疗仍然具有挑战性。近期,来自丹麦的团队开展了真实世界研究,旨在比较ICIs实施前后,一线治疗EGFR/ALK阴性晚期NSCLC患者的总生存期(OS),确定影响OS预后的因素。相关结果发表在Cancers杂志上。
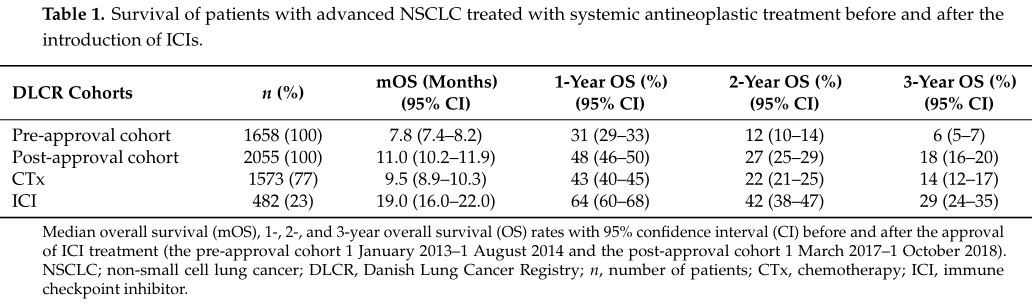
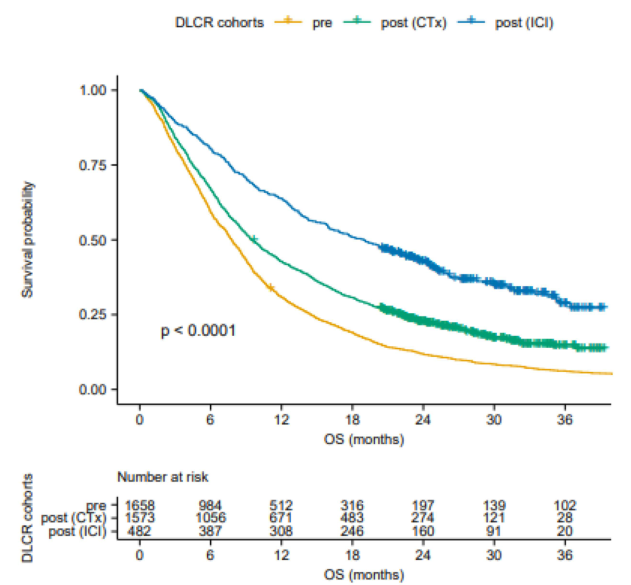
研究筛选丹麦肺癌数据库(DLCR)2013年1月1日至2018年10月1日进行一线治疗的晚期NSCLC。根据免疫检查点抑制剂(ICI)获批治疗前后,分为获批前队列(n= 1658)和获批后队列(n= 2055),后者分为DLCR-CTx(化疗)组(n= 1573)和DLCR-ICI组(n=482)。
相对于获批前队列,获批后队列的女性比例(50.2% vs. 46.9%,p = 0.05)和腺癌比例(58.8% vs. 53.3%, p < 0.0001)较高。同样,相对于DLCR-CTx组,DLCR-ICI组的女性比例较高(58.3% vs. 47.7%, p < 0.0001)。
相对于获批前队列,获批后队列的OS明显改善。获批前队列的中位OS为7.8 个月(7.4–8.2),1年、2年和3年OS率分别为31% (29–33),12% (10–14) 和6 %(5–7);而获批后队列的中位OS为11.0个月 (10.2–11.9),1年、2年和3年OS率分别为48% (46–50),27% (25–29)和 18% (16–20)。DLCR-CTx组和DLCR-ICI组的中位OS分别为9.5个月 (8.9–10.3)和19.0 个月(16.0–22.0)。两组1年、2年和3年OS率分别为43% (40–45) vs 64% (60–68),22% (21–25) vs 42% (38–47),和14 %(12–17) vs 29% (24–35)。
OS
OS
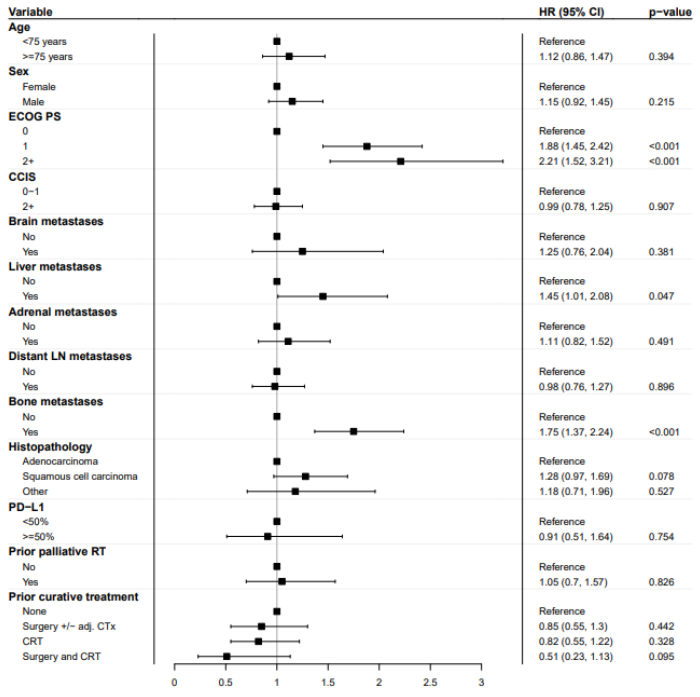
因为DLCR数据库中患者的PS,转移部位和抗肿瘤治疗细节等缺少,研究者纳入EHRs数据库相关患者的数据(n=579)。中位OS为18.3个月(95% CI 16.0 21.3);男性为15.2个月 (95% CI 13.0 18.3),女性为21.5个月 (95% CI 18.0 25.1)。PS=0患者的中位OS为28个月(95% CI 21.5 NR),而PS=1和2患者的mOS分别为14.6个月(95% CI 12.7 19.0)和12.8个月(95% CI 7.6 16.1)。BoM患者的mOS为12.0个月(95% CI 9.5 14.9),而非BoM患者的mOS为21.5个月(95% CI 19.0 24.9)。中位PFS为8.2个月(95% CI 7.2 9.3);男性为7.1个月 (95% CI 6.0 8.5),女性为8.8 个月(95% CI 7.9 11.8)。PS=0患者的mPFS为11.0个月(95% CI 8.5 13.9),而PS =1和2患者的mPFS为7.7个月(95% CI 6.4 8.8)和6.0个月(95% CI 3.3 8.7)。BoM患者的mPFS为5.7个月(95% CI 4.4 7.8),而非BoM患者的mPFS为9.4个月(95% CI 8.1 12.0)。
在多变量Cox回归分析中,PS=1 (HR = 1.86;95%CI1.44-2.39;p < 0.001)和PS≥2 (HR = 2.19;95%CI1.5-3.18;p<0.001),BoM (HR = 1.75;95%CI 1.36-2.23;p<0.001)、肝转移(HR = 1.44;95%CI 1.0-2.07;P = 0.05)是独立不良预后因素。
亚组分析
综上,研究表明,免疫检查点抑制剂(ICI)的获批明显改善EGFR/ALK阴性晚期NSCLC患者的OS。PS≥1, 骨转移和肝转移是不良预后因素。
原始出处:
Mouritzen, M.T.; Carus, A.;Ladekarl, M.; et al. Nationwide Survival Benefit after Implementation of First-Line Immunotherapy for Patients with Advanced NSCLC—Real World Efficacy. Cancers 2021, 13, 4846. https://doi.org/ 10.3390/cancers13194846
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#研究数据#
45
#SCLC患者#
42
#ERS#
39
#生存获益#
37
#真实世界#
34
#NSCLC患者#
29
#晚期NSCLC#
0
#GFR#
39
学习了
46
学习
49