Hypertension:急性卒中血栓切除术中血压与结局的关系
2020-01-14 xing.T MedSci原创
总之,在急性缺血性卒中伴大血管闭塞的患者中,MT前后的BP水平升高与不良预后相关。
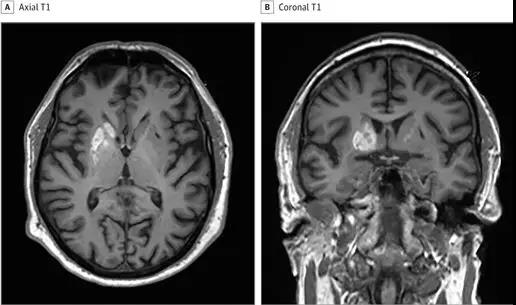
在机械性血栓切除术(MT)治疗的急性缺血性卒中合并大血管阻塞的患者中,评估血压(BP)对临床结局影响的数据十分有限。近日,心血管权威杂志Hypertension上发表了一篇研究文章,研究人员试图评估接受MT治疗的急性缺血性卒中合并大血管闭塞患者BP水平与临床结局之间的相关性。
研究人员确定了报告了MT之前、期间或之后收缩压BP(SBP)或舒张压(DBP)水平与接受MT治疗的急性缺血性卒中患者预后之间相关性的研究。研究人员进行了未经调整和调整的分析,报告了BP每增加10mmHg的比值比(ORadj)。
该分析包含了25项研究,涉及6474名患者。在3个月内死亡的患者中观察到较高的MT前平均SBP(P=0.008)和MT后最大SBP(P=0.009)水平。3个月功能独立性患者MT前(P<0.001)和MT后最大SBP水平(P<0.001)较低。在调整后的分析中,MT后最大SBP和DBP水平升高与3个月死亡率(ORadj为1.19[95%CI为1.00-1.43];I2=78%,Cochran Q检验的P值=0.001)和症状性颅内出血(ORadj为1.65[95%CI为1.11-2.44];I2=0%,Cochran Q检验的P值=0.80)相关。MT前、后平均SBP水平升高与较低的3个月功能独立性几率相关(ORadj为0.86[95%CI为0.77-0.96];I2=18%,Cochran Q检验的P值=0.30)和(ORadj为0.80[95%CI为0.72-0.89]; I2=0%,Cochran Q检验的P值=0.51)。
总之,在急性缺血性卒中伴大血管闭塞的患者中,MT前后的BP水平升高与不良预后相关。
原始出处:
Konark Malhotra.et al.Association of Blood Pressure With Outcomes in Acute Stroke Thrombectomy.Hypertension.2020.https://www.ahajournals.org/doi/10.1161/HYPERTENSIONAHA.119.14230
本文系梅斯医学(MedSci)原创编译整理,转载需授权!
版权声明:
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#切除术#
37
#TENS#
43
#PE#
41
学习
83
#急性卒中#
38
#血栓切除#
36
#血栓切除术#
33
#Hypertension#
32
卒中虽然是临床上常见病,溶栓,取栓等血管内治疗也很成熟,但是仍然有很多未知问题有待认知!
53