JCEM:正常范围上限的血清PTH水平与心血管疾病相关
2013-08-15 desperado-c dxy
越来越多的证据表明甲状旁腺功能亢进与心血管疾病发病率和死亡率风险增加有关。然而,关于正常范围血清甲状旁腺素(PTH)水平与心血管疾病(CVD)的关系所知甚少。为研究正常水平血清PTH与CVD和腹主动脉钙化(AAC)的关系,来自荷兰阿姆斯特丹自由大学医学中心的Elisabeth M Eekhoff教授及其团队进行了一项研究,发现血清PTH水平处于正常范围上限与CVD高度相关。该研究结果在线发表于20
越来越多的证据表明甲状旁腺功能亢进与心血管疾病发病率和死亡率风险增加有关。然而,关于正常范围血清甲状旁腺素(PTH)水平与心血管疾病(CVD)的关系所知甚少。为研究正常水平血清PTH与CVD和腹主动脉钙化(AAC)的关系,来自荷兰阿姆斯特丹自由大学医学中心的Elisabeth M Eekhoff教授及其团队进行了一项研究,发现血清PTH水平处于正常范围上限与CVD高度相关。该研究结果在线发表于2013年8月8日的《临床内分泌代谢杂志》(The journal of clinical endocrinology & metabolism)上。【原文下载】
该研究使用阿姆斯特丹老龄化纵向研究(LASA)的资料进行了一项基于人群的横断面研究,共纳入年龄在65–88岁的558名男性受试者和537名女性受试者,分别控制其性别、年龄、体重指数、高血压、糖尿病、高密度脂蛋白胆固醇、总胆固醇、吸烟、体力活动、饮酒、肾小球滤过率、采血的季节、钙和利尿剂的使用、血清25–羟维生素D和骨钙蛋白等混杂因素。
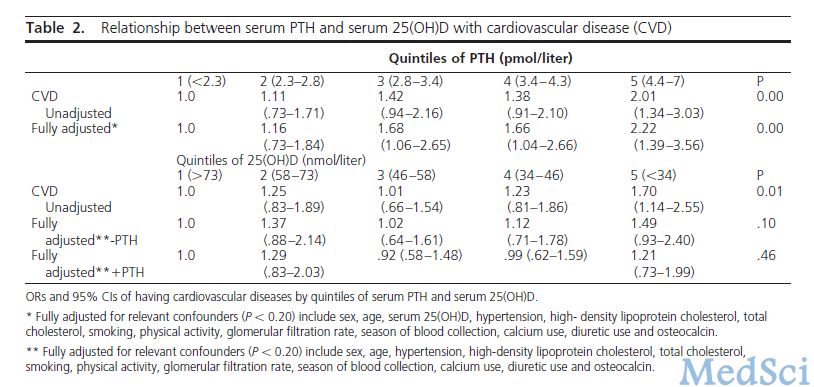
研究结果发现,多元模型显示血清PTH位于最高五分位数的受试者与位于最低五分位数的受试者相比,CVD风险显著增加。仅在男性中观察到PTH与AAC有关,且在校正混杂因素后,该相关性仍具有统计学意义。
该研究结果表明,老年人血清PTH水平处于正常范围上限与CVD高度相关,并且在老年男性中,腹主动脉钙化可对该相关性做出一定解释。
原始出处:
Buizert PJ van Schoor NM Simsek S Lips P Heijboer AC den Heijer M Deeg DJ Eekhoff EM.PTH: A NEW TARGET IN ARTERIOSCLEROSIS?J Clin Endocrinol Metab 2013 Aug 【原文下载】
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#JCE#
32
#JCEM#
20
#PTH#
24
#血管疾病#
24