Muscle Nerve:间充质干细胞治疗ALS的3期临床试验失败
2022-06-26 廖联明 MedSci原创
肌萎缩侧索硬化(ALS)是一种神经退行性疾病,其特征是皮质和脊髓运动神经元的进行性变性和丢失。神经炎症起着重要作用。目前还没有治愈ALS的方法,也没有任何治疗方法可以阻止或逆转疾病的进展。以多种疾病途
肌萎缩侧索硬化(ALS)是一种神经退行性疾病,其特征是皮质和脊髓运动神经元的进行性变性和丢失。神经炎症起着重要作用。目前还没有治愈ALS的方法,也没有任何治疗方法可以阻止或逆转疾病的进展。以多种疾病途径为靶点的细胞疗法有可能通过分泌神经保护因子和调节神经炎症和神经退行性路径来支持患病神经细胞的存活。
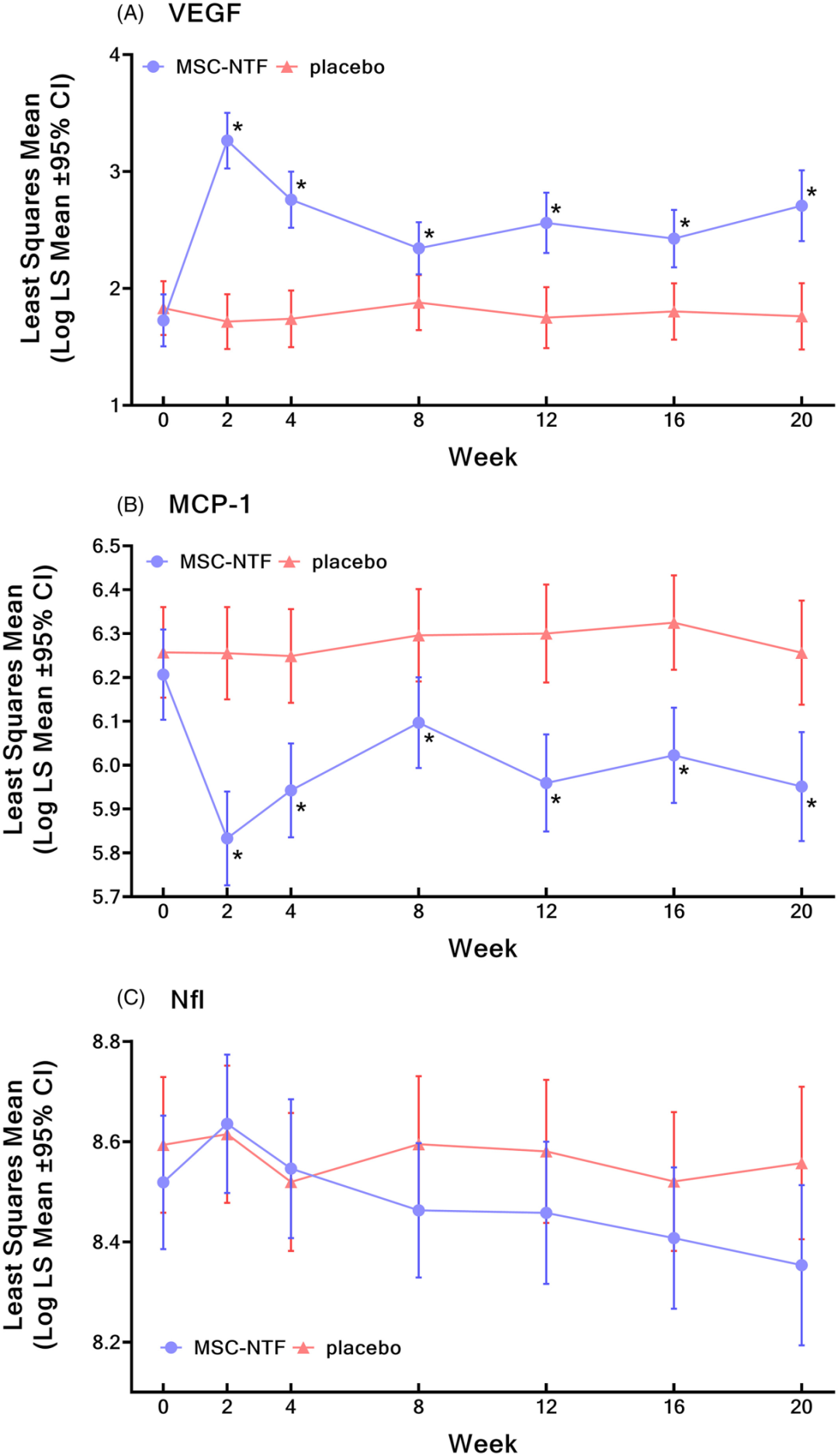
Brainstorm Cell Therapeutics研发的成人骨髓的间充质干细胞(MSC)在专有的体外条件下诱导分泌高水平的神经营养因子(MSC-NTF)。1,2期临床研究显示单次鞘内给药后MSC-NTF(代号NurOwn®)可以提高脑脊液(CSF)神经保护因子和降低神经炎性因子,MSC-NTF具有安全性和初步疗效。但3期临床试验的结果却令人失望。

BCT-002研究(NCT03280056)是一项平行组、随机、双盲、安慰剂对照研究,在美国六个学术中心进行。
在为期18周的预治疗期(包括门诊骨髓抽吸术)后,参与者在第0周、第8周和第16周接受鞘内治疗,然后进行为期12周的观察。
参与者为18-60岁,根据修订的El-Escorial标准,有实验室支持可能、可能或明确的ALS,症状发作≤24 月,修订的ALS功能评分量表(ALSFRS-R)总分 ≥ 25。允许参与者服用稳定剂量的利鲁唑。
随机分组后,参与者通过标准腰椎穿刺接受鞘内MSC-NTF(NurOwn®,由Dana Farber癌症研究所或希望之城制造)或安慰剂。
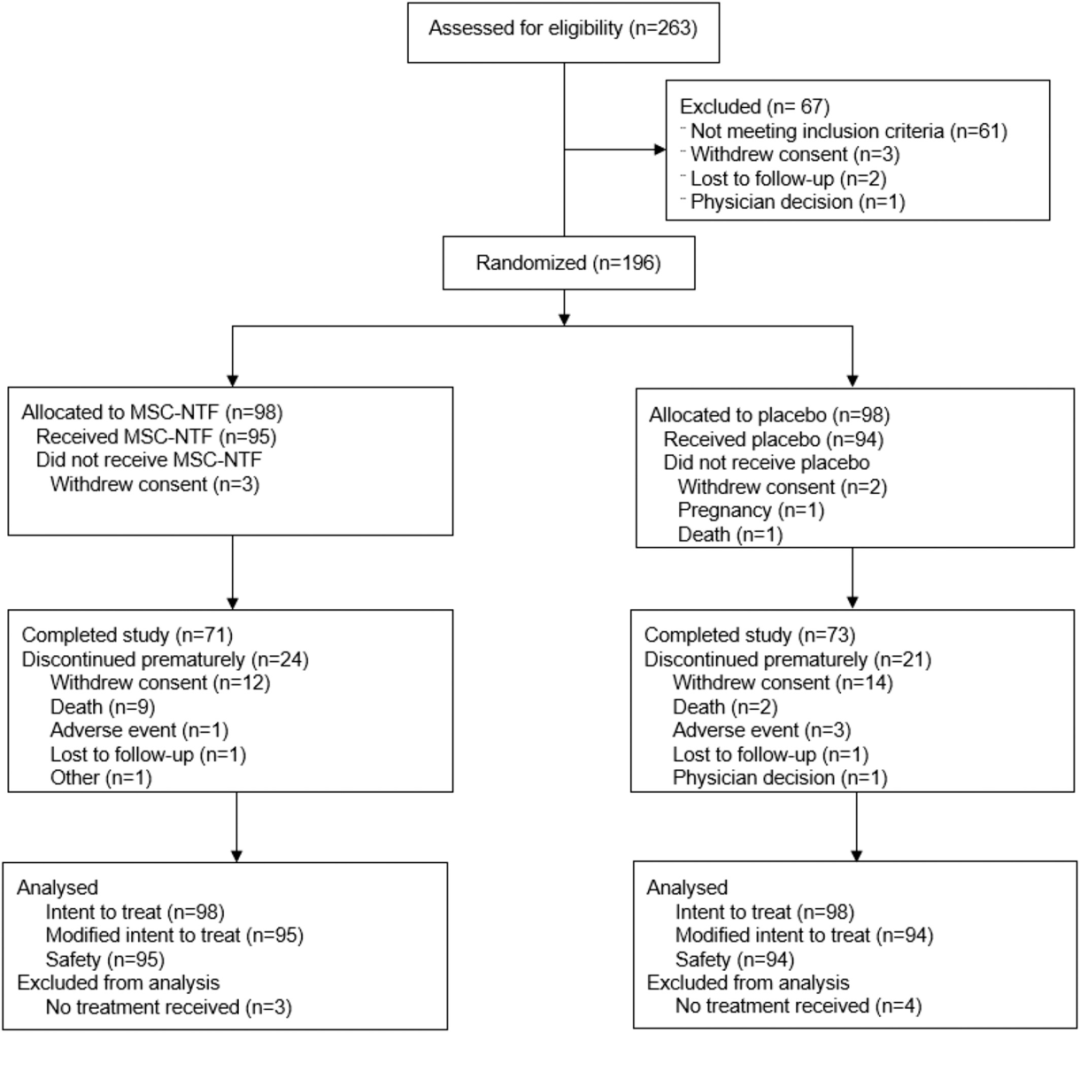
2017年8月至2020年9月,263名ALS患者接受了资格筛查;196人被随机分配到治疗组,189人接受至少一次治疗。七名参与者没有接受治疗。共有45名参与者过早中止了研究。
治疗组之间的基线特征总体上是平衡的
在研究过程中,各治疗组在任何时间点的临床实验室值、生命体征、体检结果和心电图结果无显著差异。在研究期间,16名参与者死亡。没有与治疗相关的死亡。总的来说,MSC-NTF耐受性良好,没有安全问题。
研究结束后33%的MSC-NTF组患者和28%的安慰剂组患者达到临床反应标准(优势比=1.33,P=0.45),两组没有差异;因此,未达到主要终点。
然而亚组表明,与安慰剂相比,病情较轻的MSC-NTF参与者可能保留了更多的功能,值得进一步研究。
与其他晚期ALS试验相比,本研究参与者的病情更为严重,这可能具有稀释效应,降低了在整个研究人群中显示治疗效果的能力。
这项研究由Brainstorm Cell Therapeutics资助。这项研究还得到了两项资助:加利福尼亚再生医学研究所(CIRM,CLIN2-09894)和ALS协会和”我是ALS”的资助。
原始出处:
Cudkowicz ME, Lindborg SR, Goyal NA, Miller RG, Burford MJ, Berry JD, Nicholson KA, Mozaffar T, Katz JS, Jenkins LJ, Baloh RH, Lewis RA, Staff NP, Owegi MA, Berry DA, Gothelf Y, Levy YS, Aricha R, Kern RZ, Windebank AJ, Brown RH Jr.A randomized placebo-controlled phase 3 study of mesenchymal stem cells induced to secrete high levels of neurotrophic factors in amyotrophic lateral sclerosis.Muscle Nerve. 2022 Mar;65(3):291-302. doi: 10.1002/mus.27472
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#muscle#
61
#3期临床#
58
#间充质干细#
52
继续
52
#3期临床试验#
42
不容易啊。
36
值得学习
38
不错,学习了。
49
好文章,值得一读。
52