JAHA:围手术期代谢产物与先天性心脏病新生儿不良手术结局相关
2022-08-12 MedSci原创 MedSci原创
在新生儿心脏手术中,围手术期代谢产物与术后结局和改善的临床模型结局相关。仅术前代谢物水平可改善风险模型,并为优化围手术期治疗提供了依据。
新生儿心脏手术的临床危险因素并不能完全反映结局的差异。近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,研究人员对接受体外循环开展心脏手术的新生儿血浆进行靶向代谢组学分析,以确定其与临床结局之间的相关性。

研究人员纳入了2012年至2016年期间接受皮质类固醇治疗且经体外循环开展先天性心脏病手术的149例新生儿的样本和临床变量。

研究人员在皮肤切开前、体外循环后即刻、术后12小时采集受试者血液样本。结局包括复合发病率/死亡率(死亡、体外膜氧合、心脏骤停、急性肾损伤和/或肝损伤)和心脏复合(体外膜氧合、心脏骤停或乳酸水平升高)、肝损伤和急性肾损伤。目标代谢物水平由高分辨率串联液相色谱和质谱测定。研究人员使用主成分和回归分析来评估代谢谱和患者结局之间的关联,并创建了两个模型:基本临床模型和基本模型+代谢物。
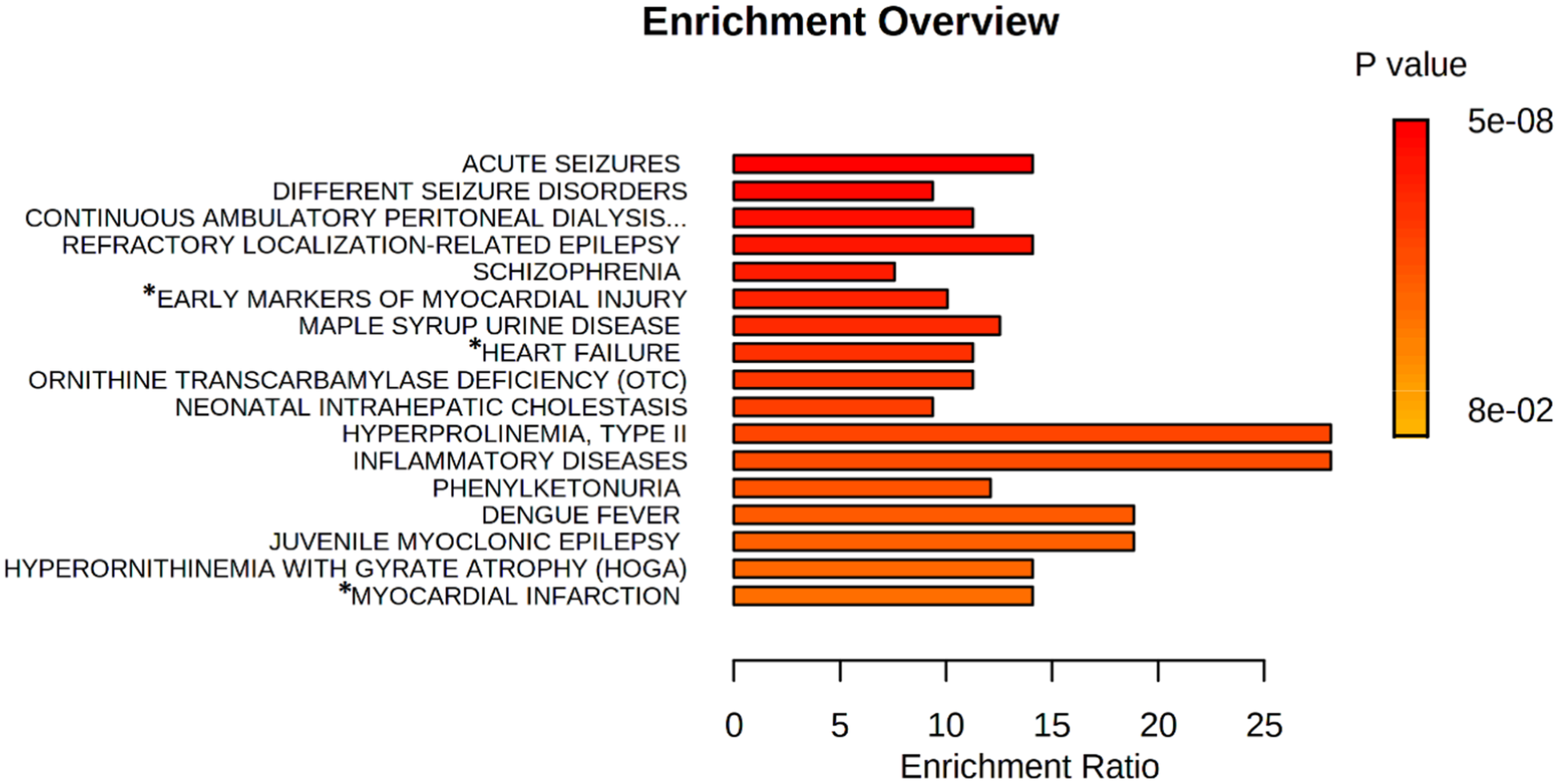
在检测的193个代谢物中,有40个被检测和定量。第一个主成分,主成分1,主要由术前代谢产物组成,与符合发病率/死亡率、心脏复合事件和肝损伤结局显著相关。在回归模型中,个体代谢物也改善了复合发病率/死亡率、心脏复合事件和肝损伤结局的模型性能。重要的疾病途径包括心肌损伤(假发现率为0.00091)和心力衰竭(假发现率为0.041)。
在新生儿心脏手术中,围手术期代谢产物与术后结局和改善的临床模型结局相关。仅术前代谢物水平可改善风险模型,并为优化围手术期治疗提供了依据。
原始出处:
Jessica Heibel.et al.Perioperative Metabolites Are Associated With Adverse Neonatal Congenital Heart Disease Surgical Outcomes.JAHA.2022.https://www.ahajournals.org/doi/full/10.1161/JAHA.121.024996
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#手术期#
47
#AHA#
0
#先天性#
55
#代谢产物#
48