AP&T: I、III和IV型胶原蛋白相关的血清学标志物与狭窄性和穿透性克罗恩病疾病进展有关
2022-08-12 xuyihan MedSci原创
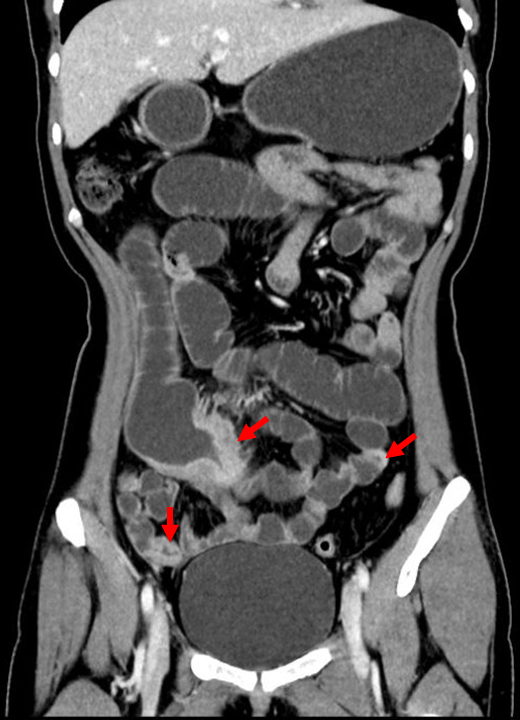
克罗恩病是一种慢性的肠道炎症,可以从口腔、肛门、全消化道发生,往往最为常见的好发部位是在回盲部以及小肠,它的主要临床表现是腹痛、腹块、瘘管形成、肠梗阻。
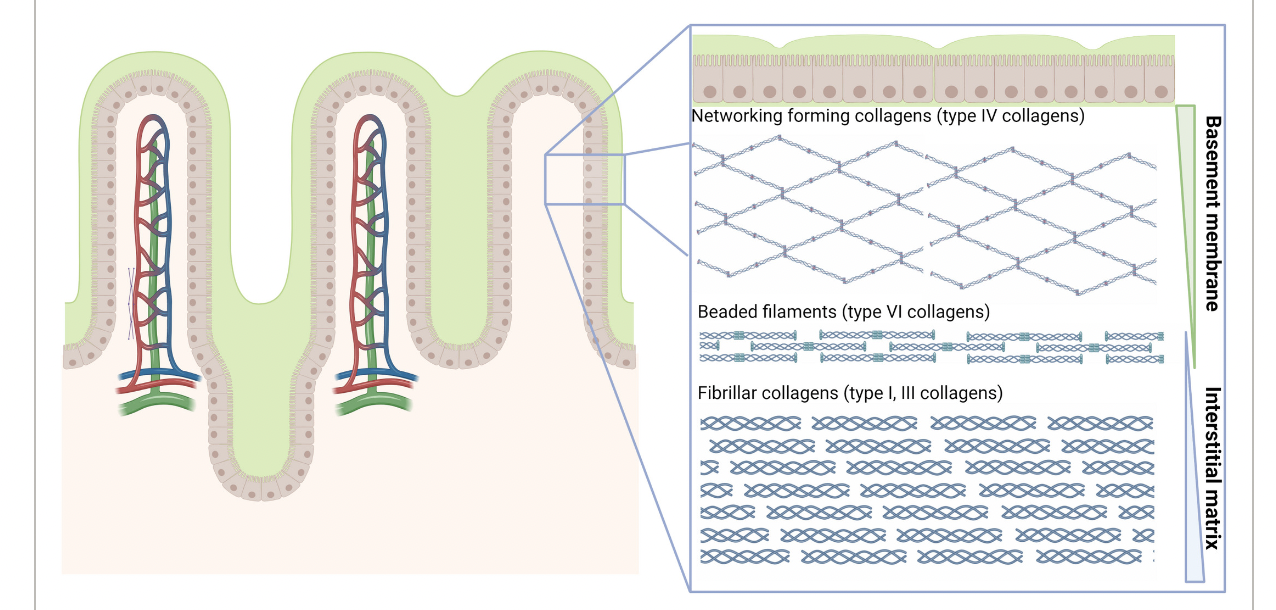
克罗恩病 (CD) 是一种主要影响胃肠道 (GI) 的慢性炎症性肠病,主要发病机制可能与遗传易感个体的肠道微生物组有关。长期疾病活动可能会使患者的疾病发展为狭窄(即肠狭窄)和穿透性(即肠瘘、脓肿或穿孔)疾病表型,肠粘膜下层富含细胞外基质(ECM)蛋白,包括胶原蛋白,它们对于维持肠组织的上皮完整性和结构以及拉伸强度非常重要。ECM可分为两层,基底膜(BM)和间质基质(IM)。BM中最丰富的胶原蛋白是IV型胶原蛋白,而I型和III型胶原蛋白是IM中最丰富的胶原蛋白,它们与肠上皮细胞直接相关。纤维化被认为是这些疾病并发症的主要病理生理机制,这是由于过度的ECM沉积(主要是胶原蛋白)以及慢性炎症和伤口愈合受损导致的异常重塑的结果。本项研究旨在评估循环胶原蛋白形成和降解片段是否可以作为CD患者蒙特利尔疾病行为亚类的鉴别生物标志物。
研究人员收集了101名CD患者的血清样本,其中III/IV 型胶原蛋白形成(PRO-C3、PRO-C4)和基质金属蛋白酶(MMP)或颗粒酶-B(GrzB)介导的 I、III、IV 和 VI 型胶原蛋白降解产物分别为C1M、C3M、C4M,C4G、C6Ma3。101名CD患者中蒙特利尔分型分别为B1:n = 37;B2:n = 27;B3:n = 37),同时本项研究还纳入了96名对照健康人群。所有患者均随访直至最后一次门诊就诊,以监测狭窄/穿透性疾病的进展和复发以及手术干预的发生。
研究结果显示C1M、C3M 和 C4M在狭窄性疾病患者(蒙特利尔B2)中显着降低,并可以很好地将非狭窄、非穿透性 (B1) 或穿透性 (B3) 疾病患者区分开来(p< 0.001)。 同样,IV型胶原形成/降解 (PRO-C4/C4M) 比率表现出很高的辨别能力(B1/B2:AUC = 0.90;B1/B3:AUC = 0.87,p < 0.001)。同时研究人员还发现较高的C1M和C4G基线水平与穿透性疾病进展的风险增加相关(C4G:风险比 [HR] 1.71 [1.05–2.81],p< 0.05)。
本项研究证实I、III 和 IV 型胶原蛋白的降解产物增加以及IV型胶原蛋白的过度形成与狭窄的CD密切相关。I型和IV型胶原蛋白片段显示出穿透性疾病进展风险的预测潜力。这些生物标志物可能成为检测和预测狭窄和穿透性 CD 的宝贵工具。
原始出处:
Arno R. Bourgonje. et al. Serological biomarkers of type I, III and IV collagen turnover are associated with the presence and future progression of stricturing and penetrating Crohnʼs disease. Alimentary Pharmacology & Therapeutics.2022.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#疾病进展#
56
#III#
42
#标志物#
46
#血清学#
50
#胶原蛋白#
65