JAHA:外周动脉疾病患者心衰与结局的关联
2021-06-01 MedSci原创 MedSci原创
外周动脉疾病 (PAD) 和心力衰竭 (HF) 均与不良结局独立相关。原发性PAD患者与新发HF相关的危险因素尚未明确。此外,HF是否与PAD患者结局之间存在相关性也尚未明确。
外周动脉疾病 (PAD) 和心力衰竭 (HF) 均与不良结局独立相关。原发性PAD患者与新发HF相关的危险因素尚未明确。此外,HF是否与PAD患者结局之间存在相关性也尚未明确。

近日,心血管疾病领域权威杂志JAHA上发表了一篇研究文章,该研究对随机分配至替格瑞洛或氯吡格雷治疗的有症状PAD患者HF相关危险因素与结局之间的关系。根据入组时是否伴有HF对患者进行分层。Cox模型用于明确HF与结局之间的关联。在随访期间,研究人员使用了单独的Cox模型来明确与HF发生相关的危险因素。

伴有HF的PAD患者冠状动脉疾病的发生率是没有HF患者的两倍多。伴有HF的PAD患者发生主要不良心血管事件(风险比 [HR]为1.31;95%CI为1.13-1.51)和全因死亡(HR为1.39;95%CI为1.19-1.63)的风险显著增加。
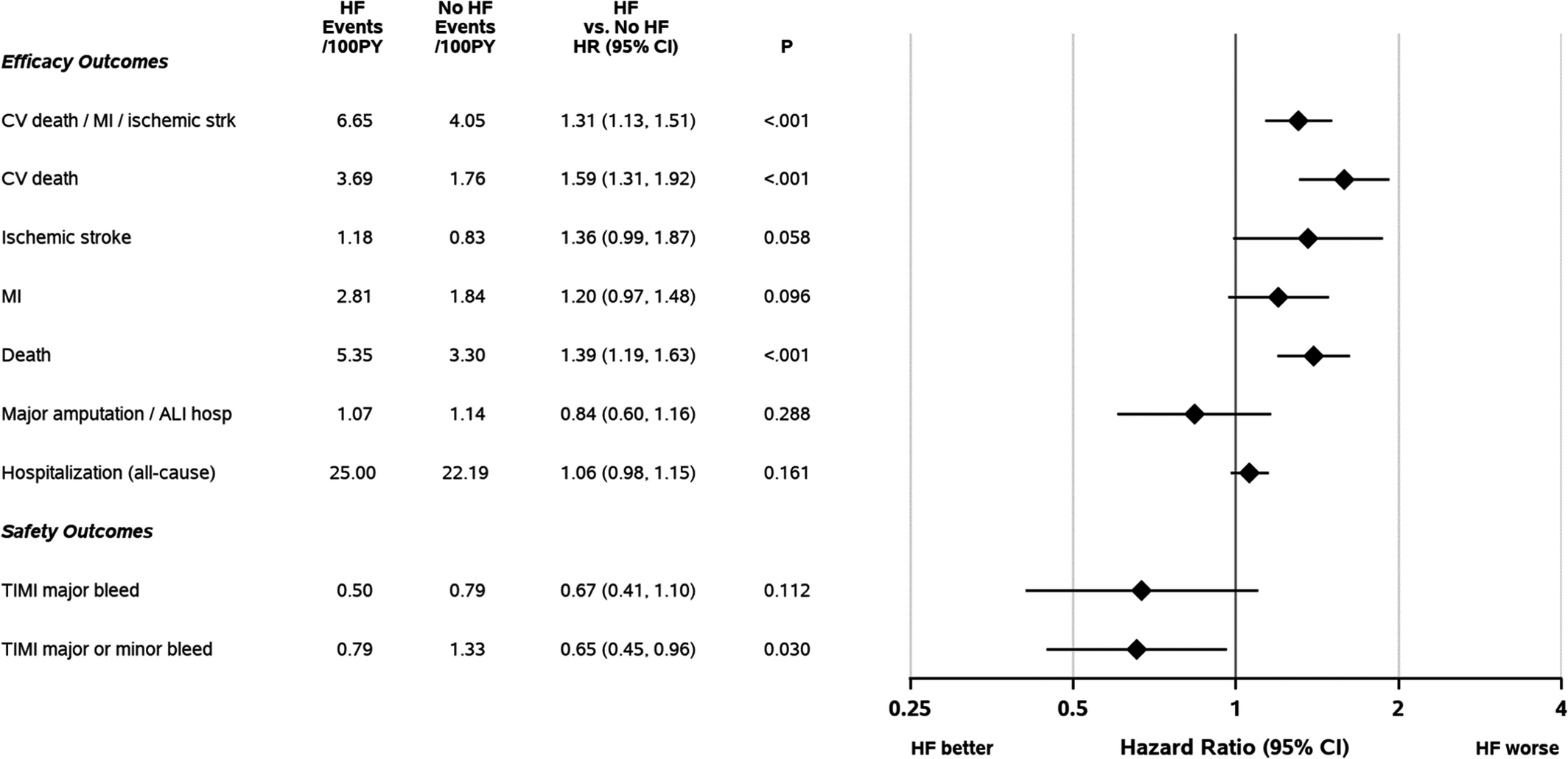
心衰与结局的关系
在PAD患者中,伴有HF与出血减少显著相关(HR为0.65;95%CI为0.45-0.96)。与HF发生相关的特征包括年龄≥66(HR为1.29;95%CI为1.18-1.40)、糖尿病(HR为1.85;95%CI为1.41-2.43)和体重(双向相关,≥76 kg,HR为0.77;95%CI为0.64-0.93;<76 kg,HR为1.12;95%CI为1.07-1.16)。
由此可见,伴有HF的PAD患者冠状动脉疾病的发生率很高,并且重大心血管不良事件和死亡的风险也很高。这些数据支持PAD患者,尤其伴有HF时,需要积极治疗动脉粥样硬化疾病。
原始出处:
Marc D. Samsky.et al.Association of Heart Failure With Outcomes Among Patients With Peripheral Artery Disease: Insights From EUCLID.J AM HEART ASSOC.2021.https://www.ahajournals.org/doi/full/10.1161/JAHA.120.018684
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#疾病患者#
40
#AHA#
37
#外周动脉#
42
好文章共享
53