Nat Cancer:JBJ-09-063:非小细胞肺癌治疗的潜在EGFR变构抑制剂
2022-04-27 xiaozeng MedSci原创
肺癌是全球癌症相关死亡的主要原因之一,非小细胞肺癌(NSCLC)占所有肺癌的85%。
肺癌是全球癌症相关死亡的主要原因之一,非小细胞肺癌(NSCLC)占所有肺癌的85%。EGFR(表皮生长因子受体)是一种跨膜蛋白,隶属于酪氨酸激酶(TK)受体的ERBB家族,由其他三个密切相关的成员ERBB2、ERBB3和ERBB4组成。
既往研究显示,ERBB家族在基本的细胞功能中起着至关重要的作用,其能够调节细胞增殖、分化、存活和迁移等多种下游信号通路的激活。诱导受体组成型激活、扩增或过表达的突变会引起不受控制的细胞增殖的发生,这是癌症的一大标志。
EGFR突变是NSCLC中最常见致癌驱动因素之一,而EGFR也被鉴定为潜在的靶向治疗候选靶标。既往的研究显示,EGFR的小分子酪氨酸激酶抑制剂(TKI)疗法对于EGFR 突变肺癌患者具有一定的治疗效果,但通常会伴随着耐药性的出现。
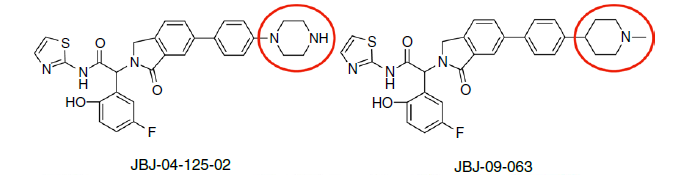
JBJ-09-063的化学结构
EGFR变构抑制剂被发现能够与现有的ATP竞争性的EGFR TKI结合到不同的EGFR位点上,被认为是克服EGFR突变患者治疗耐药性的潜在治疗策略。
在该研究中,研究人员鉴定了一种更为有效的EGFR突变选择性变构抑制剂JBJ-09-063,并探究其功效。研究人员发现,JBJ-09-063对EGFR TKI敏感且对耐药模型有效,包括具有EGFR T790M和C797S突变的模型。进一步研究发现,包括EGFR L747S突变在内的EGFR能够通过与其他ERBB家族成员进行同源或异源二聚化而产生对JBJ-09-063的耐药性,但该作用对ATP竞争性EGFR TKI并无耐药性。这也是限制JBJ-09-063治疗功效的分子和生物决定因素。
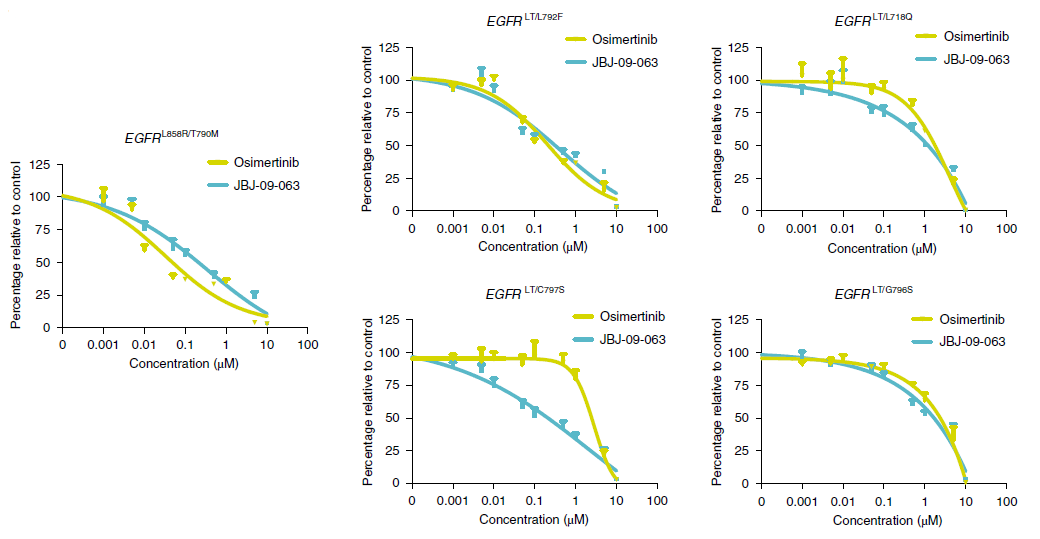
JBJ-09-063的给药效果
总而言之,该研究结果揭示了JBJ-09-063作为单一药物或与EGFR TKI联用的潜在临床功效,并确定了EGFR突变肺癌的更有效的治疗策略。
原始出处:
To, C., Beyett, T.S., Jang, J. et al. An allosteric inhibitor against the therapy-resistant mutant forms of EGFR in non-small cell lung cancer. Nat Cancer (14 April 2022).https://doi.org/10.1038/s43018-022-00351-8.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#Nat#
31
#肺癌治疗#
50
#抑制剂#
36
#非小细胞#
0
#GFR#
37