DCR: CD4/CD8比率可以作为感染 HIV患者中高度肛门发育不良和肛门癌高风险的依据
2021-06-30 MedSci原创 MedSci原创
在美国,退伍军人中的HIV感染率是所有人群中比例最高的。因此,在美国,医生建议所有感染 HIV 的退伍军人筛查肛门发育不良以及肛门癌症的发生情况。
在美国,退伍军人中的HIV感染率是所有人群中比例最高的。因此,在美国,医生建议所有感染 HIV 的退伍军人筛查肛门发育不良以及肛门癌症的发生情况。但是肛门检查具有侵入性以及依从性较差的缺点,因此,本项研究旨在探究晚期肛门疾病(高度不典型增生和肛门癌)的患病率,并确定 CD4/CD8 比率是否与此相关。
这是一项针对感染 HIV的退伍军人的回顾性队列研究,研究人员将处于肛门部不典型增生晚期的患者与非晚期肛门病理患者进行比较。Logistic 回归模型用于估计患癌疾病的几率。评估了每个队列中最低(最低点)CD4/CD8 和最接近的 CD4/CD8 比率。
本项研究共纳入了2267名退伍军人。15% 有肛门病变(112 人为晚期疾病(37 人为癌症,75 人为高级别瘤变),222 人为非晚期疾病)。晚期疾病患者与非晚期患者的CD4/CD8最低点和最接近比率较低(0.24 对 0.45(p < 0.001)和 0.50 对 0.88(p < 0.001))。在调整后的模型中,最低点或最接近比率增加 1 个单位可降低晚期疾病的风险(OR = 0.19(95% CI,0.07–0.53);p < 0.001;OR = 0.22(95% CI,0.12–0.43) ; p < 0.001)。使用最小敏感性分析,可以使用 0.42 的临界最低点比率来进行风险分层。
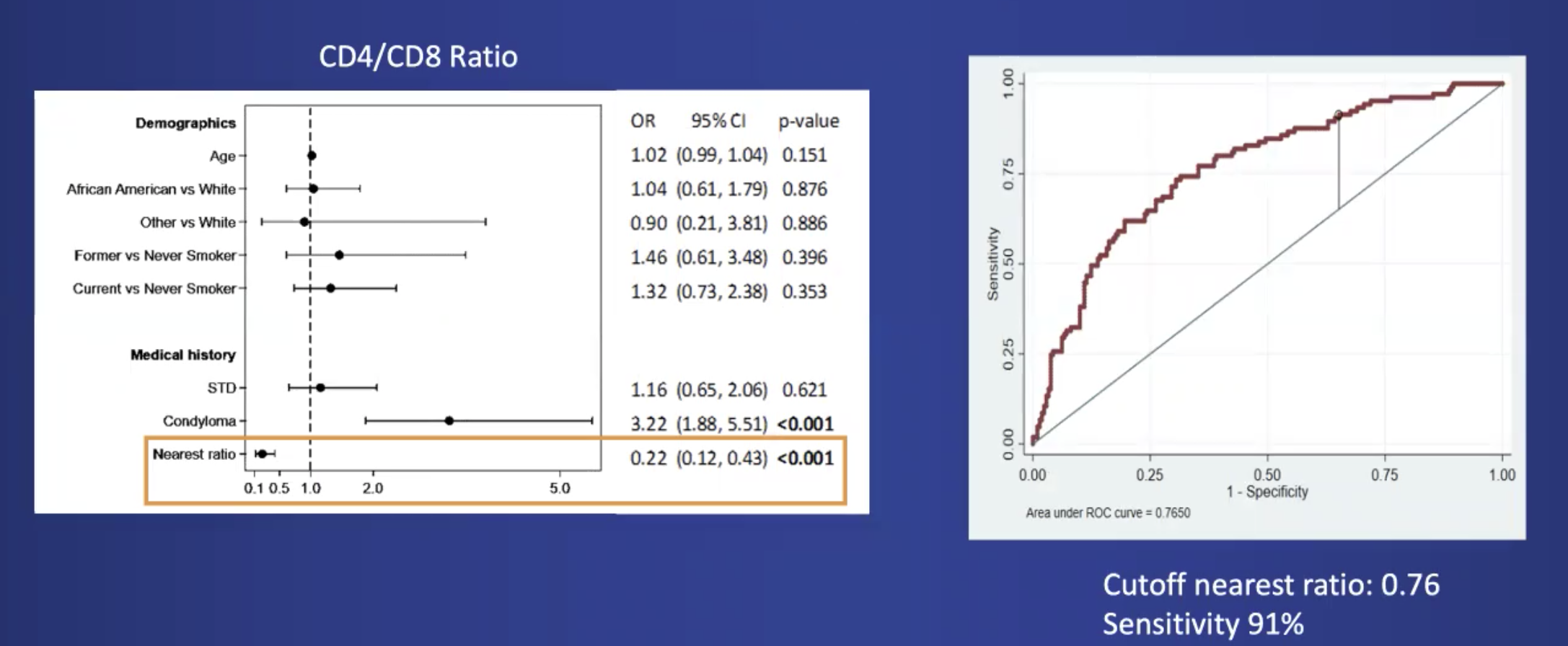
图:CD4/CD8与HIV患者中高度肛门发育不良和肛门癌高风险的相关性
本项研究发现5%的 HIV 阳性人群存在晚期肛门癌变疾病。该队列中晚期疾病的一个强有力的预测指标是 CD4/CD8 比率。使用 CD4/CD8 进行风险分层有可能减少对低风险患者进行频繁的侵入性检查。
原始出处:
Sanger, Cristina. Et al. Prevalence of High-Grade Anal Dysplasia and Anal Cancer in Veterans Living With HIV and CD4/CD8 Ratio as a Marker For Increased Risk.Diseases of the Colon & Rectum.2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#HIV患者#
39
#CD4#
55
#肛门#
55
#高风险#
40
#发育#
35
#发育不良#
28
#CD8#
33