DAPT的出血管理策略——冠心病双联抗血小板治疗中国专家共识解读
2021-06-30 “Clinic門诊新视野”公众号 “Clinic門诊新视野”公众号
DAPT已经被临床医生广泛认可,对于接受PCI治疗的冠心病患者而言,双联抗血小板治疗(DAPT)是PCI围术期及术后长期管理中无法绕开的重要治疗手段之一;而在通过DAPT预防缺血事件的同时,出血风险也
DAPT已经被临床医生广泛认可,对于接受PCI治疗的冠心病患者而言,双联抗血小板治疗(DAPT)是PCI围术期及术后长期管理中无法绕开的重要治疗手段之一;而在通过DAPT预防缺血事件的同时,出血风险也不可避免地随之提高,这会给临床治疗带来一些挑战。近日,由解放军北部战区总医院韩雅玲院士牵头,中华医学会心血管病学分会组织中华医学会心血管病分会动脉粥样硬化与冠心病学组及介入心脏病学组、中国医师协会心血管内科医师分会血栓防治专业委员会及冠心病与动脉粥样硬化专业委员会联合制定的《冠心病双联抗血小板治疗中国专家共识》正式发布!作为我国在该领域的首部专家共识,该文献在参考中外最新循证医学证据及欧美相关指南推荐的基础上,结合我国国情,对接受PCI治疗的不同患者群体的DAPT治疗予以了规范性推荐。
高出血风险患者人群的DAPT策略制定
PCI术后出血高危因素主要包括:高龄、女性、肾功能不全、慢性心力衰竭、血小板减少或抗血小板治疗后抑制过度、贫血、低体重指数、合用口服抗凝药(Oral anticoagulants,OAC)等。在面对这类特殊患者群体时,临床医师务必要使用专门用于指导DAPT疗程制定的风险评分(如:PRECISE-DAPT评分和DAPT评分),从而确保术后抗栓治疗的有效性与安全性。
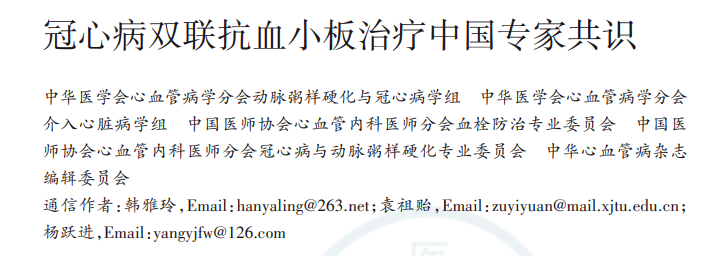
一般而言,PRECISE-DAPT评分≥25分的患者人群属于高出血风险,应适当缩短DAPT疗程。我国最新公布的《冠心病双联抗血小板治疗中国专家共识》建议(图1):对于接受PCI的患者,若PRECISE-DAPT评分≥25分,可考虑3~6个月的短期DAPT(IIb,A);对于PCI术后DAPT 12个月内未发生任何事件的患者,若DAPT评分<2分,可考虑12个月的标准疗程DAPT(IIb,A)。
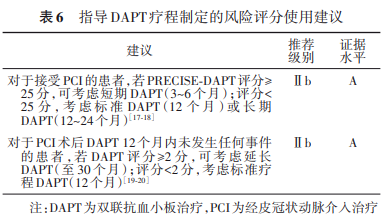
图1. 指导DAPT疗程制定的风险评分使用建议
有效降低出血风险与相关并发症的策略探索
在利用各种评分系统精准地筛选和评估高出血风险患者人群的同时,临床上也在不断思考能在DAPT期间最大程度地减少出血风险的有效措施。早在2015年,MATRIX研究[2]就指出,相较于传统的股动脉入路,经桡动脉入路行PCI治疗的患者术后30天内MACE事件(包括:心血管性死亡、MI和卒中)以及严重出血事件发生率均显着更低;而另一项名为TIFU的非干预性观察队列研究[3]则发现,低剂量阿司匹林可显着降低BARC定义的出血风险且不增加MACE事件风险。另外,由于上消化道出血是长期抗血小板治疗过程中最常见的出血并发症,使用PPI可减轻阿司匹林治疗患者的消化道损伤并预防出血及复发出血[4]。但在应用PPI时,部分PPI 通过CYP2C19竞争性抑制氯吡格雷的抗血小板作用,可能影响其临床疗效,因此与氯吡格雷联用时,推荐使用受 CYP2C19 影响较小的 PPI(如泮托拉唑、雷贝拉唑等),不建议氯吡格雷与奥美拉唑或埃索美拉唑同时使用。
也正是基于以上循证医学证据的支持,最新发布的《冠心病双联抗血小板治疗中国专家共识》中明确推荐:建议在配备桡动脉径路手术专家的情况下,有限选择桡动脉入路进行冠脉造影和PCI(I,A);建议接受DAPT的患者使用阿司匹林的剂量范围为75~100 mg/d(I,A);建议在DAPT基础上联合使用PPI(I,B)。
非心脏外科手术前停药对出血风险的影响
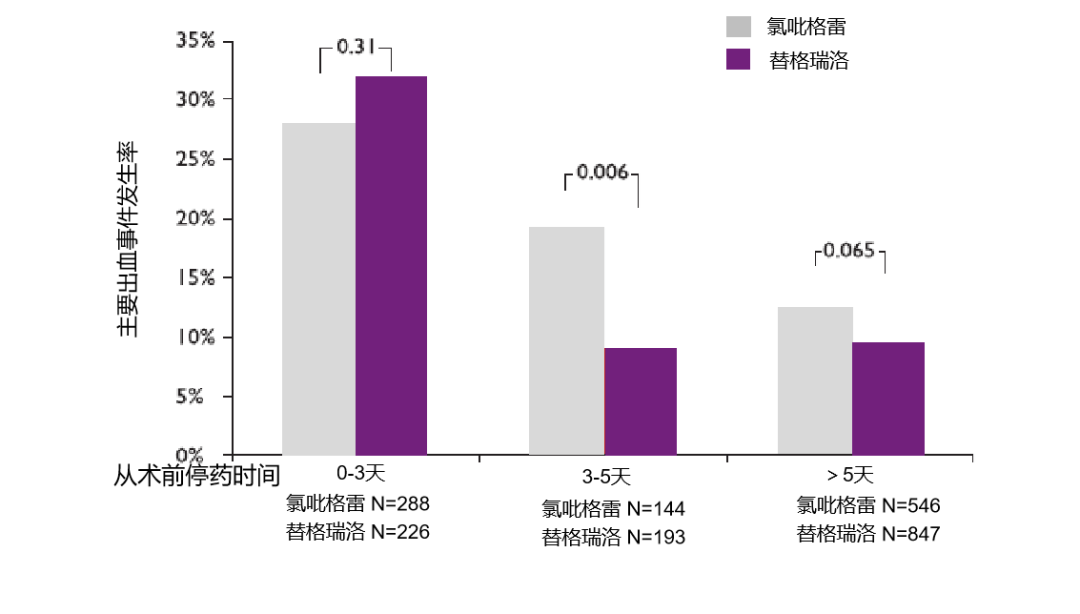
对于接受PCI治疗的患者而言,提前停用抗血小板药物一直是临床上预防术中出血过多的常规策略,而提前停药时间过长显然会增加缺血事件的发生风险,故非心脏外科手术前究竟应提前多长时间停药,始终是临床医师反复权衡的重点。2017年,Valgimigli等人于European Heart Journal发表的一项研究[5]发现(图2),非心脏外科手术前停用P2Y12类抗血小板药物的时间越长(>5天),患者的主要出血事件风险就越低;而非心脏外科手术前3~5天内停药,强效P2Y12受体抑制剂(替格瑞洛)相较于氯吡格雷的术后主要出血事件发生率显着更低,且具有显着统计学差异(P=0.006)。
图2. PCI术前停药时间对主要出血事件发生率的影响
当然,从该研究结果亦可看出,强效P2Y12受体抑制剂(替格瑞洛)提前3~5天与提前>5天停药的主要出血事件发生率基本一致;而对于氯吡格雷而言,提前>5天停药较提前3~5天停药的出血风险明显更低;可见,强效P2Y12受体抑制剂(替格瑞洛)所需的停药时间更短,因停药而产生的缺血风险也将更低。最新的《冠心病双联抗血小板治疗中国专家共识》[1]亦给出了类似推荐:针对非心脏外科手术期间的DAPT,对于替格瑞洛治疗的患者,应至少在术前3天考虑停用;对于氯吡格雷治疗的患者,至少术前5天停用(IIa,B)。
抗血小板药物致出血后的DAPT方案管理与处理措施
尽管临床上给出了多重预防出血事件的建议或推荐,但这类事件的发生总是在所难免。针对使用DAPT并已致出血情况的患者人群[1]:如是微小出血,则可继续DAPT治疗;如为轻度出血,可考虑缩短DAPT持续时间或降阶治疗,尤其是再次出血时;如发生中度出血或严重出血,应考虑停用DAPT,改为SAPT(更倾向于保留P2Y12受体抑制剂);如发生危及生命的出血事件,则应立即停用所有抗栓药物,而一旦出血停止,须重新对是否需要DAPT或SAPT进行评估,更倾向于保留P2Y12受体抑制剂,尤其是上消化道出血时(图3)。
图3. 合用或未合用OAC患者接受DAPT治疗期间发生出血的推荐处理措施
对于抗血小板药物致出血后的DAPT方案管理,《冠心病双联抗血小板治疗中国专家共识》也给出了详细建议:立刻权衡出血和缺血风险并重新评估DAPT,并待病情稳定后,尽快恢复抗血小板治疗(3~5天后恢复P2Y12受体抑制剂,5~7天后恢复阿司匹林)。针对高血栓风险的出血,建议继续使用低剂量的阿司匹林维持抗栓,待出血稳定后再重新加用P2Y12受体抑制剂;针对于中等血栓风险的出血,建议控制出血后(最好3天内)重新给予低剂量阿司匹林,权衡缺血出血风险后再重新启动P2Y12受体抑制剂。PCI术后3个月内的出血,出血停止后重新启动DAPT不超过3个月,其后改为单一抗血小板药物;PCI术后3个月以上的出血,建议降低抗栓强度,给予一种抗血小板药物(阿司匹林或P2Y12受体抑制剂)。
总 结
在DAPT治疗过程中,准确评估患者的出血与缺血风险、恰当选择P2Y12受体抑制剂类型与剂量、慎重调整DAPT疗程时长,并及时针对出血事件予以有效的干预治疗,方能实现抗栓治疗获益的最大化。现有临床研究证据已证实经桡动脉入路、低剂量阿司匹林应用以及提前停用抗栓药物等措施可帮助降低出血风险事件的发生率,我国最新发布的《冠心病双联抗血小板治疗中国专家共识》同样给出了类似建议,但总体而言,在DAPT方案的制定过程中,临床医师还是应始终结合患者的个体情况作出适应性调整,避免拘泥于指南文献的“条条框框”,方能取得最好的抗栓治疗效果。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#管理策略#
0
#中国专家共识#
49
#专家共识#
46
#双联抗血小板#
44
#DAPT#
46
#双联抗血小板治疗#
61