J Hepatol:8mmTIPS支架疗效与风险如何?
2017-05-13 MedSci MedSci原创
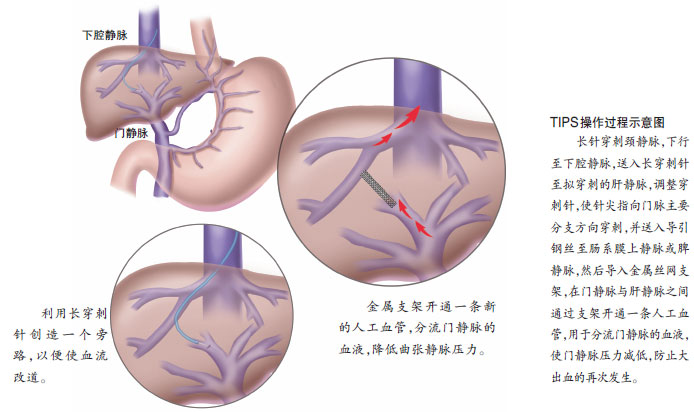
目前,由于缺乏足够的证据,关于经颈静脉肝内门体分流术(TIPS)的支架优选直径的建议指南还未发表。因此,该项目评估了8 mm支架是否能实现和10 mm支架在减少肝性脑病(HE)发生率,提升肝功能相同效果的分流功能。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#TIPS#
34
感谢分享一下!!
71
学习一下觉得非常好
72
#iPS#
34
#EPA#
32