GUT: MELD评分以及Child-Pugh 分级高的患者应早期行TIPS术
2018-11-19 MedSci MedSci原创
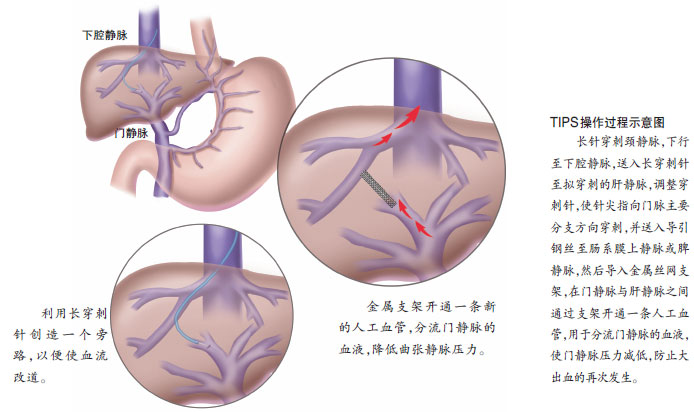
早期放置经颈静脉肝内门体分流术(TIPS)可提高肝硬化和急性静脉曲张出血(AVB)的高风险患者(Child-Pugh B加内镜下活动性出血或Child-Pugh C)的生存率。然而,早期TIPS标准可能会高估大部分患者的死亡风险,并且早期TIPS赋予此类患者的生存益处是否做够满意令人质疑。本项研究旨在探明何种患者适合TIPS手术。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#child#
26
#ILD#
24
#Child-Pugh#
32
#TIPS#
34
#iPS#
27
#MELD#
31