Clin Cancer Res:CEACAM7是CAR-T细胞治疗胰腺导管腺癌的有效靶点
2021-01-23 MedSci原创 MedSci原创
胰腺导管腺癌(PDAC)是第四最常见的实体瘤相关死亡原因,其5年存活率不足5%。
胰腺导管腺癌(PDAC)是第四最常见的实体瘤相关死亡原因,其5年存活率不足5%。CEACAM7(CGM2)是一个目前研究比较少的CEA家族成员,该家族蛋白具有多种功能,在恶性肿瘤中常见失调。Deepak等人推测CEACAM7可能是CAR T细胞疗法治疗PDAC的一个合适的靶点,对此进行了研究,并制备了CEACAM7靶向CAR T细胞以验证这一假说。
Deepak等人确定了CEACAM7是CEA家族蛋白中的一员,其表达局限于结肠和胰腺,是PDAC潜在的CAR T细胞靶点。研究人员检测了PDAC肿瘤切片以及患者来源的PDAC细胞中CEACAM7的表达,构建了靶向CEACAM7的CAR T细胞,并利用体内外模型评估了CEACAM7 CAR T细胞的抗肿瘤效果。
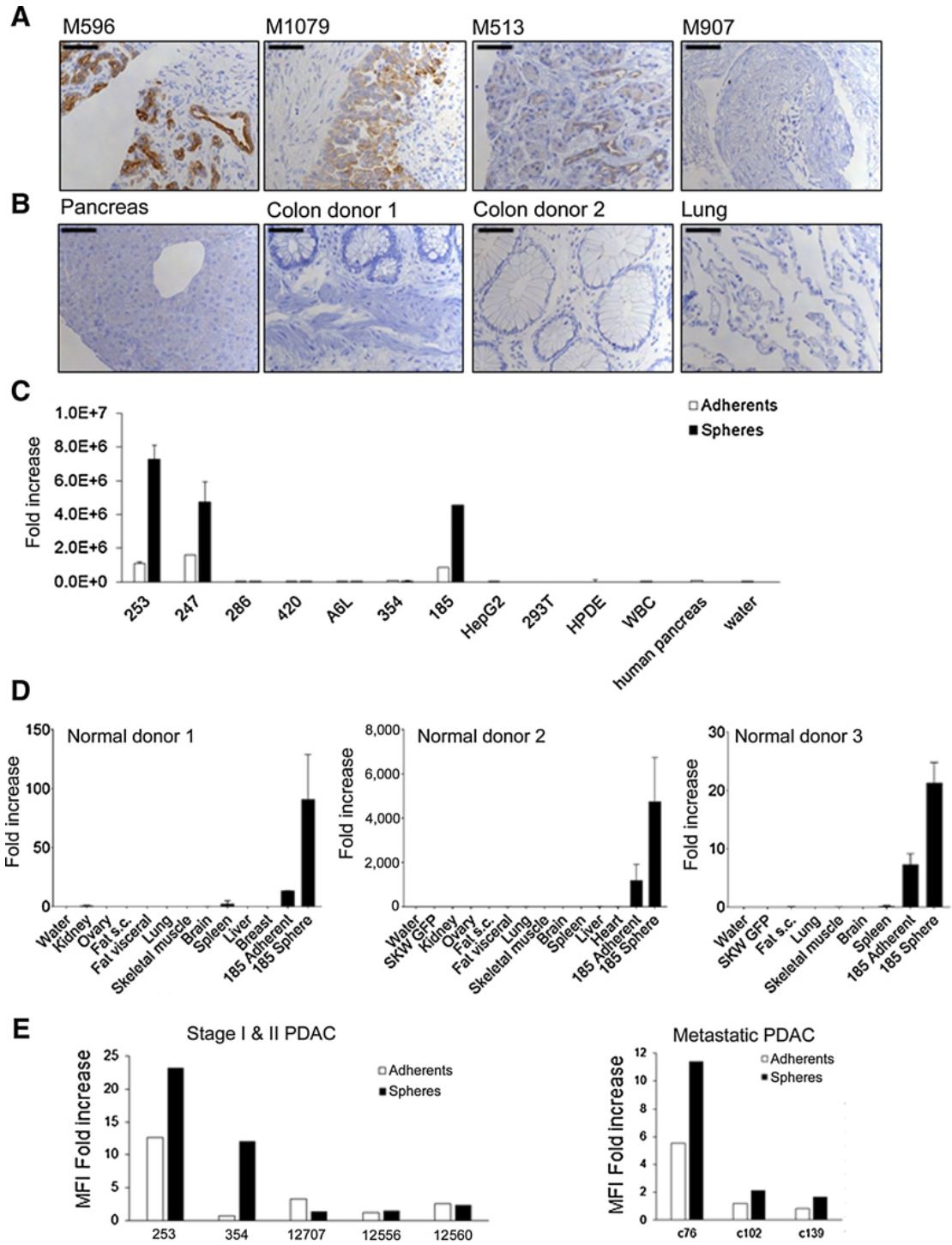
CEACAM7在各类组织中的表达
结果显示,CEACAM7在PDAC肿瘤的一个大亚群中表达,在所有被测试的正常组织中表达很低或检测不到。CEACAM7也在从患者来源的肿瘤中分离出的PDAC原代细胞中表达,还在肿瘤干细胞富集的亚群中高表达。
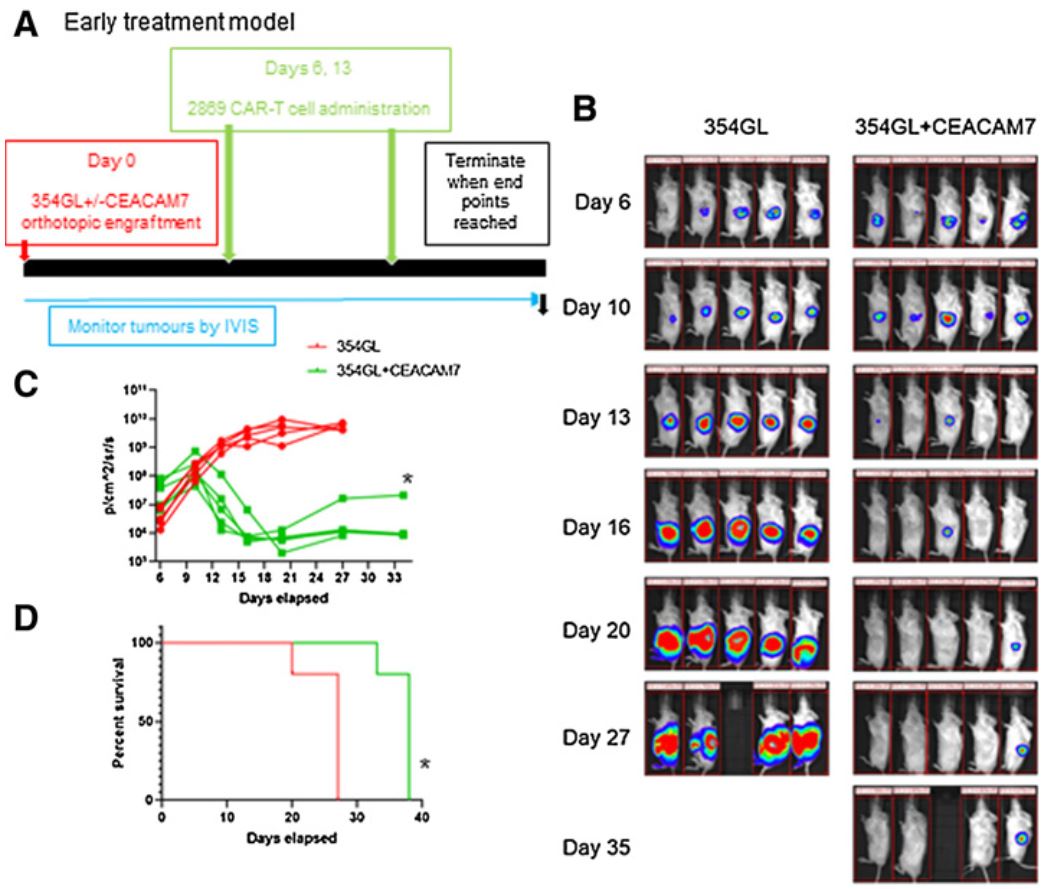
靶向CEACAM7的CAR T细胞的抗肿瘤活性
靶向CEACAM7的CAR T细胞能够靶向抗原表达的肿瘤细胞,并可延缓患者来源的异种移植瘤的生长。
综上,该研究表明,CEACAM7确定为PDAC的潜在治疗靶点,而且构建了靶向CEACAM7的CAR T细胞,并验证了其抗PDAC的疗效。
原始出处:
Raj Deepak,Nikolaidi Maria,Garces Irene et al. CEACAM7 Is an Effective Target for CAR T-cell Therapy of Pancreatic Ductal Adenocarcinoma. Clin Cancer Res, 2021, 10.1158/1078-0432.CCR-19-2163.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#CAR-#
39
#ACA#
32
#CAM#
44
#CEA#
35
学习
101
靶向CEACAM7的CAR T细胞能够靶向抗原表达的肿瘤细胞,并可延缓患者来源的异种移植瘤的生长。
76
#胰腺导管腺癌#
116
很不错
80
学习了
67
好文章
24