eLife:脑损伤激活胶质细胞产生神经元研究获新进展
2019-08-29 黄辛 何静 科学网
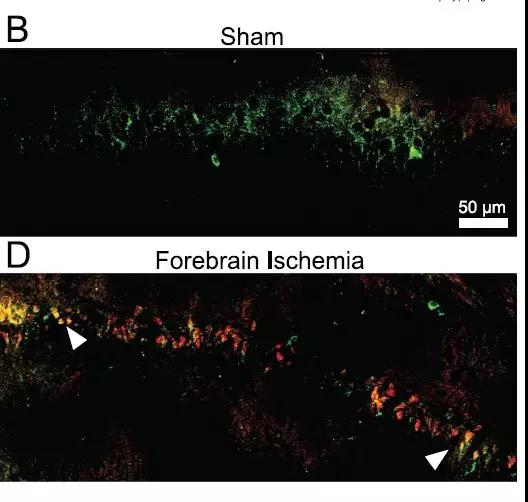
胶质细胞是人脑中数量最多的细胞。但是,在人脑创伤情况下,胶质细胞的潜在反应和作用还很不清楚?中国科学院脑科学与智能技术卓越创新中心何杰研究组开展的研究,回答了两个关于胶质细胞如何响应脑损伤的关键性问题:损伤激活的胶质细胞如何进入细胞周期?损伤激活的胶质细胞如何选择产生胶质细胞还是神经元?近日,eLife在线发表这项研究论文。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#Life#
40
#eLife#
30
学习了,学习了
85
#胶质细胞#
34
#损伤#
38
向科研人员致敬!!!
96