Front Oncol: PD-L1抑制剂durvalumab用于局部进展期食管和胃食管连接处腺癌术后辅助治疗的疗效:II期临床研究
2021-09-18 yd2015 MedSci原创
研究表明,PD-L1抑制剂durvalumab用于局部进展期食管和胃食管连接处腺癌术后辅助治疗具有改善无复发生存期的临床获益,并且跟PD-L1水平有一定相关。
大多数可切除的局部晚期食管和胃食管连接处(GEJ)腺癌(AC)患者接受同期放化疗(CRT)后进行手术。新辅助CRT治疗后,大多数患者仍不能达到病理完全缓解(pCR),而且这部分患者复发率高。因此,有研究团队开展II期临床研究,评估在局部晚期食管腺癌和胃食管连接处腺癌的患者,新辅助CRT后行R0切除术,手术标本中证明残留疾病,然后进行durvalumab辅助治疗,评估疗效和安全性。相关结果发表在Frontiers in Oncology杂志上。

该研究为II期临床研究(NCT02639065),主要终点为1年无复发生存期(RFS)。次要终点是治疗后durvalumab辅助治疗的安全性和耐受性。探索研究的终点包括RFS与PD-L1表达、HER-2表达和肿瘤免疫细胞群的相关性。
37名患者被纳入研究。大多数(64.9%)为病理阳性淋巴结。最常见的治疗相关不良事件为疲劳(27%)、腹泻(18.9%)、关节痛(16.2%)、恶心(16.2%)、瘙痒(16.2%)、咳嗽(10.8%),AST/ALT/胆红素升高(10.8%)。3例(8.1%)患者发生3级免疫介导不良事件。

治疗相关不良事件
中位随访时间为17.7个月(1.7–24.3)。1年RFS率为73% (95% CI, 56-84%),2年RFS率为50% (95% CI, 33–66%);中位RFS为21个月(95% CI, 14 40.4个月)。 1年OS率为94%,2年OS率为71%,中位OS为30.7个月(95% CI, 19.9-40.4)。
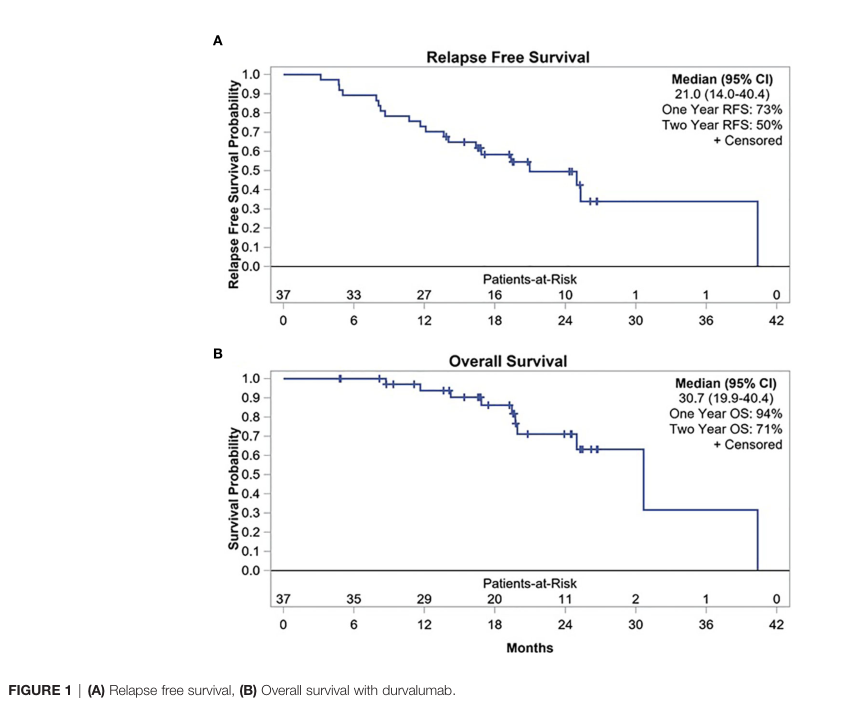
RFS和OS
与食管腺癌患者相比,GEJ AC患者的1年RFS率在数值上有一定优势 (83% vs 63%, p = 0.1534)。同样,GEJ AC患者的中位RFS较食管AC患者在数值上更长(25个月vs. 16.8个月,p = 0.4282)。
37例患者中19例(51.4%)有PD-L1 CPS≥1, 7例(18.9%)有PD-L1 CPS≥10。与PD-L1阴性患者相比,PD-L1阳性患者的1年RFS率有数值上优势,CPS≥10患者中 (100% vs. 66.7%, p = 0.1551)和CPS≥10患者中(84.2% vs. 61.1%, p = 0.1510)。与HER-2阴性患者相比,HER-2阳性患者的1年RFS率 (85.7% vs. 70%, p = 0.6471)和中位RFS (40.4 vs. 21个月,p = 0.5436)均有数值上的优势,但是没有统计学差异。
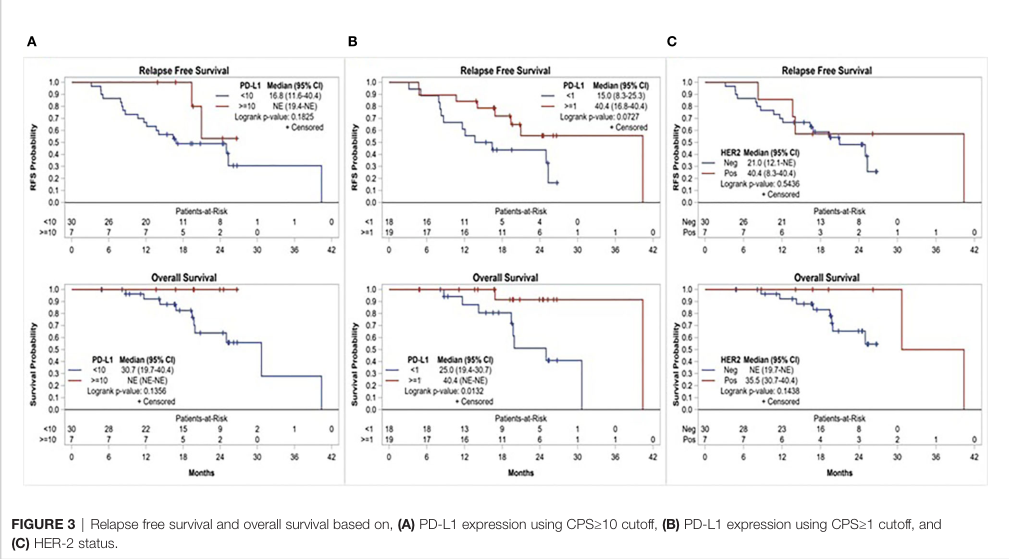
不同PD-L1水平,HER2状态的RFS
综上,研究表明,PD-L1抑制剂durvalumab用于局部进展期食管和胃食管连接处腺癌术后辅助治疗具有改善无复发生存期的临床获益,并且跟PD-L1水平有一定相关。
原始出处:
Mamdani H, Schneider B, Perkins SM, et al. (2021) A Phase II Trial of Adjuvant Durvalumab Following Trimodality Therapy for Locally Advanced Esophageal and Gastroesophageal Junction Adenocarcinoma: A Big Ten Cancer Research Consortium Study.Front. Oncol. 11:736620.doi: 10.3389/fonc.2021.736620.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#Oncol#
30
#II期临床研究#
52
#术后辅助治疗#
48
#胃食管#
0
#进展期#
60
#抑制剂#
31
#I期临床#
40
#PD-L1抑制剂#
40
#mAb#
35
#PD-L1#
47