Radiology:对于烟雾病搭桥术后血管重建的评价,只知道DSA还远远不够!
2021-04-28 shaosai MedSci原创
烟雾病是一种病因不明的、以双侧颈内动脉末端及大脑前动脉、大脑中动脉起始部慢性进行性狭窄或闭塞为特征,并继发颅底异常血管网形成的一种脑血管疾病。
烟雾病是一种病因不明的、以双侧颈内动脉末端及大脑前动脉、大脑中动脉起始部慢性进行性狭窄或闭塞为特征,并继发颅底异常血管网形成的一种脑血管疾病。由于这种颅底异常血管网在脑血管造影图像上形似“烟雾”,故称为“烟雾病”。
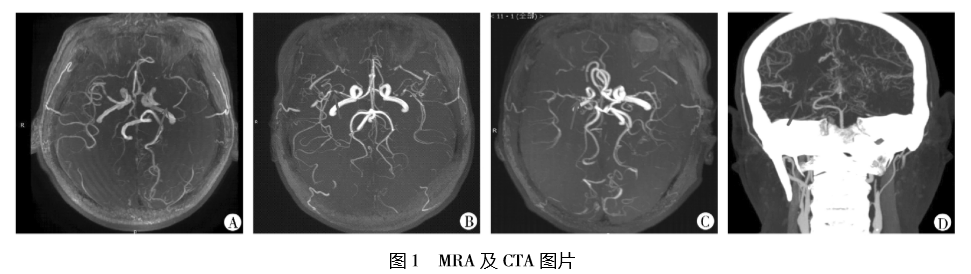
现阶段,直接及间接吻合血管重建术是临床公认的唯一有效的防止疾病进一步进展的治疗方式。在成人患者中,结合间接和直接的浅表颞动脉-大脑中动脉(MCA)吻合术是最常用的术式之一。血管重建术后,必须监控患者旁路的开放情况和评估血管化状态的变化。数字减影血管造影(DSA)是评价血管造影结果的参考标准。术后血管造影结果通常根据Matsushima等级进行评估,分为A(超过三分之二的MCA供血区域由旁路替代)、B(三分之一到三分之二)以及C(少于三分之一)。然而,DSA是一个十分耗时的侵入性检查手段,因此有并发手术相应并发症的可能性。
动脉自旋标记(ASL)灌注磁共振成像是一个可在不需要注射外源造影剂的情况下,提供脑血流量信息的非侵入性影像学手段。在烟雾病中,ASL可用于评估侧支血管、脑血管反应性以及监测手术血运重建后的灌注变化。最近,超选择性(SS) ASL技术已经多项研究被证明可以通过对每个责任动脉的SS标记来提供每个脑血管的区域灌注成像。在烟雾病中,该技术可用于监测旁路开放和评估血运重建区域情况。
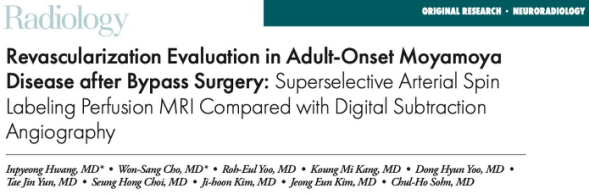
近日,发表在Radiology杂志的一项研究比较了DSA与SS-ASL灌注MRI对成年烟雾病患者直接和间接旁路联合手术后血运重建区域的成像效果,为烟雾病的进一步诊断及治疗方案的制定提供了有价值的参考意见。
对2017年6月至2019年11月间在同一家机构诊断为烟雾病并在手术后6个月接受DSA和SS-ASL检查的患者进行了回顾性评估。在10个Alberta卒中计划早期CT评分(ASPECTS)位置进行了血运重建区域和侧枝等级的主观评分。对接受术前和术后SS-ASL检查亚组的灌注状态变化进行了评估。采用加权κ统计分析交叉一致性。
本研究纳入了33例患者(平均年龄39岁±12岁[标准偏差];20名女性)的共37个半球。血管重建术区域分级的交叉一致性较强(加权κ = 0.70;95%置信区间[CI]: 0.37, 1.00)。所有血管在10个ASPECTS位置的术后侧支分级的总体交叉一致性显著(加权κ = 0.77;95%置信区间:0.74,0.80)。对于使用DSA作为参考测试的同侧颈外动脉在10个ASPECTS位置(总共370个位置)提供的术后侧支的存在,SS-ASL的敏感性为92%(199个位置中的183个;95%置信区间:87%,95%)、特异性为83% (142 / 171;95% CI: 77%,88%)。灌注状态变化的总体交叉一致性中等(加权κ = 0.59;95%置信区间:0.54,0.65)。
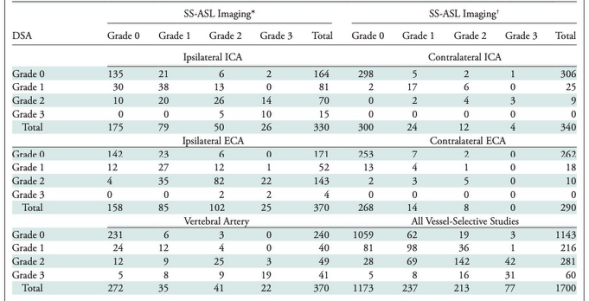
表1 SS-ASL灌注MRI与DSA之间的10个ASPECTS位置中侧支血管分级交叉一致性的列联表。

表2 以DSA作为参考测试,通过ASPECTS位置评价SS-ASL成像识别同侧外颈动脉的侧支血流的诊断性能。
本研究表明,超选择性动脉自旋标记(ASL)技术可以准确、无创地评价烟雾病患者旁路手术后的血管重建范围。此外,它也可用于评价搭桥手术前和后血管供应区域的变化。综上所述,SS-ASL可作为一种监测烟雾病患者在直接或间接旁路手术后的血运重建区域和灌注区域的变化的非侵入性的辅助手段,为临床对烟雾病患者的治疗及管理提供了有价值的参考意见。
原文出处:
Inpyeong Hwang,Won-Sang Cho,Roh-Eul Yoo,et al.Revascularization Evaluation in Adult-Onset Moyamoya Disease after Bypass Surgery: Superselective Arterial Spin Labeling Perfusion MRI Compared with Digital Subtraction Angiography.DOI:10.1148/radiol.2020201448
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#搭桥#
44
#DSA#
0
#评价#
33
#搭桥术#
53
厉害
72