Eur Urol Oncol:前列腺活检更佳方法的选择
2021-04-25 AlexYang MedSci原创
虽然磁共振成像(MRI)-靶向活检(TBx)相对于系统性活检(SBx)能更好地检测前列腺癌(PCa),但相对于单独的Bx方法,两种方法的结合能提高临床显著PCa的检测。然而,联合Bx要让患者接受更多的
虽然磁共振成像(MRI)-靶向活检(TBx)相对于系统性活检(SBx)能更好地检测前列腺癌(PCa),但相对于单独的Bx方法,两种方法的结合能提高临床显著PCa的检测。然而,联合Bx要让患者接受更多的活检核心,并对临床上不显著的PCa进行更多的检测。

最近,有研究人员确定了活检前的前列腺MRI是否可以确定哪些男性可以放弃联合Bx而不存在遗漏临床显著PCa(csPC)的风险。
研究人员对具有MRI可见的前列腺病变的男性进行了TBx和SBx的联合检查。研究的主要结果是TBx和SBx对≥2级和≥3级PCa的检出率,并按前列腺成像-报告和数据系统(PI-RADS)评分进行分层。结果发现,在PI-RADS 5 病例中,几乎所有的csPCs都是通过TBx检测出来的,因为增加SBx后,只检测到2.5%的GG≥2的癌症。然而,在PI-RADS 3-4病例中,增加SBx检测到的csPCs大大多于单独的TBx(7.5% vs 8%)。相反,相对于SBx(7.8%),TBx对PI-RADS 2病变男性中csPC的检测增加不多(2%)。
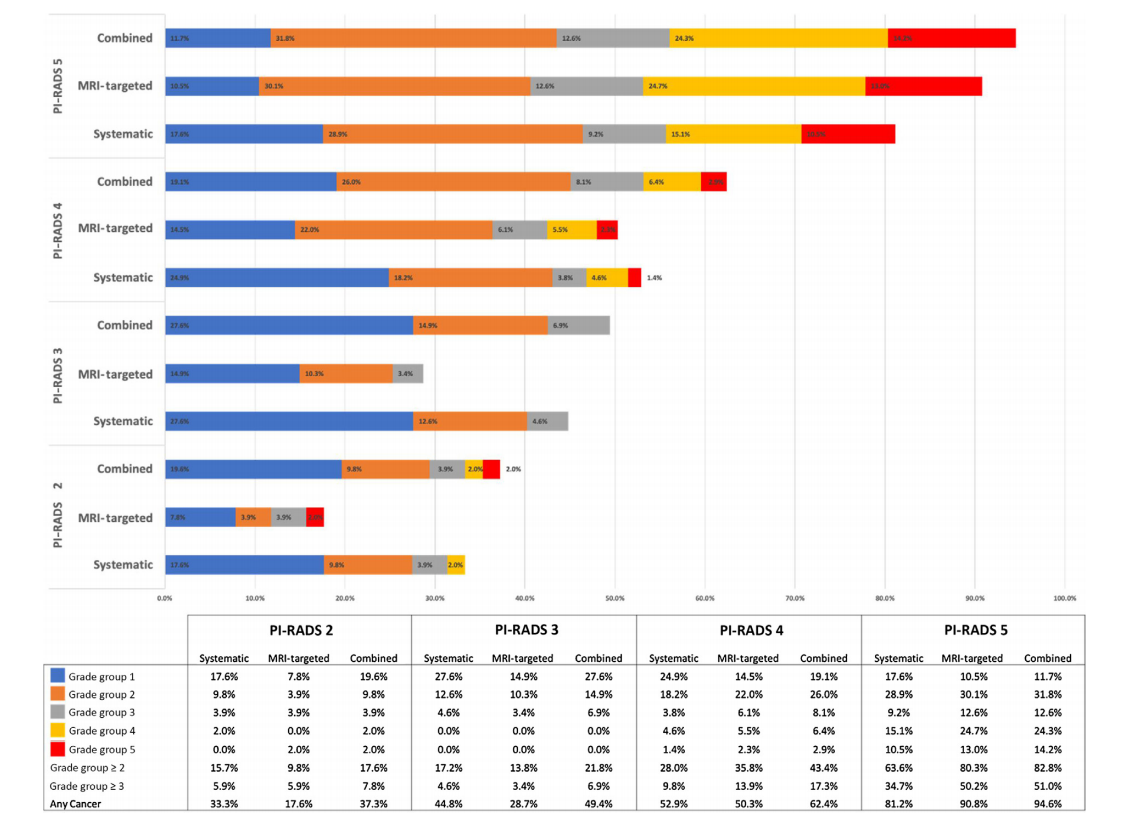
PI-RADS的癌症检出率和活检方法
最后,研究人员指出,虽然联合Bx增加了MRI可见前列腺病变男性的csPC检测,但这种效果主要限于PI-RADS 3-4病变。对PI-RADS 5的男性采用TBx,对PI-RADS 3-4的男性采用联合Bx的策略,可以避免对有PI-RADS 5病变的男性进行过多的活检,同时降低了csPC遗漏风险(1%)。
原始出处:
Michael Ahdoot , Amir H Lebastchi , Lori Long et al. Using Prostate Imaging-Reporting and Data System (PI-RADS) Scores to Select an Optimal Prostate Biopsy Method: A Secondary Analysis of the Trio Study. Eur Urol Oncol. Apr 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#前列腺活检#
41
#Oncol#
35
MRI对于提高CS的PCa检出有用
53
感谢分享
54
#活检#
34
学习一下
67
感谢分享
57
谢谢梅斯分享这么多精彩信息
46