Prostate:Vinculin通过调节肿瘤细胞的入侵、迁移和增殖来协调前列腺癌的进展
2021-03-23 AlexYang MedSci原创
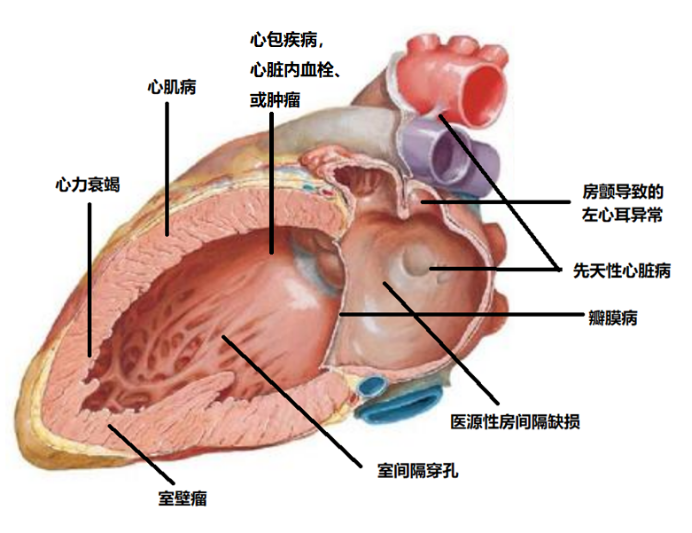
前列腺癌(PCa)是导致男性死亡的主要原因,仍旧需要进一步开发有效治疗PCa的治疗方法。
前列腺癌(PCa)是导致男性死亡的主要原因,仍旧需要进一步开发有效治疗PCa的治疗方法。

最近,有研究人员调查了vinculin(VCL)在PCa体外和体内进展中的潜在作用。
研究人员基于TCGA数据库调查了VCL启动子的甲基化水平。通过qRT-PCR、Western blot分析和免疫荧光证实了VCL基因表达的敲除效果。此外,研究人员还使用了鬼笔环肽染色法检测了PCa细胞的形态学变化;还将肿瘤细胞注射到BALB/c裸鼠右侧产生的皮下异种移植模型,调查了VCL在体内肿瘤生长中的作用。结果表明,PCa中VCL启动子的甲基化水平随着年龄和结节转移的进展而显著下调。shRNA能够明显降低VCL的表达。重要的是,VCL的敲除显著改变了细胞形态;抑制了PCa细胞的迁移、侵袭和移动,并抑制了PCa细胞在体外克隆形成和生存能力。此外,VCL的下调能够抑制体内肿瘤的生长。
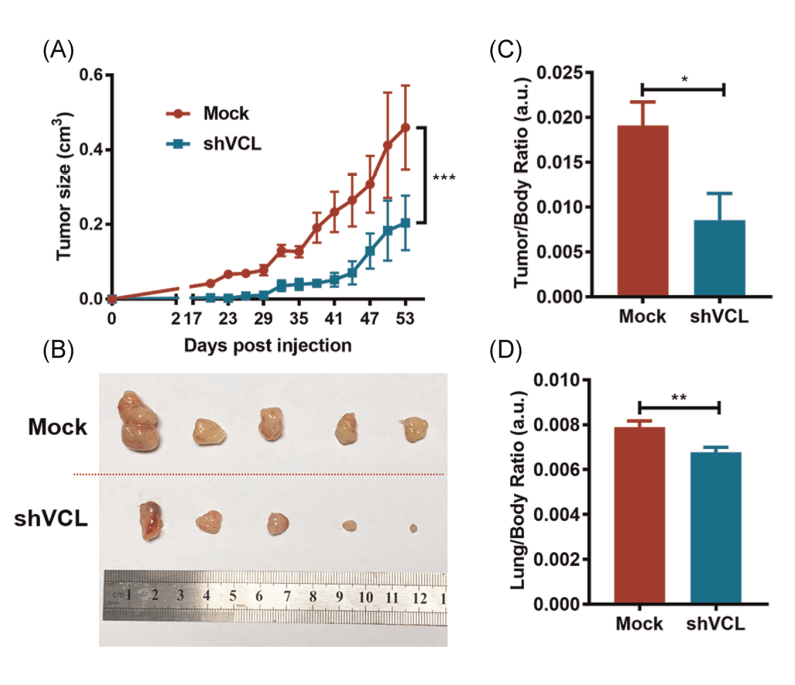
shVCL能够显著的抑制异种移植模型中肿瘤的生长
最后,研究人员指出,他们的研究全面评估了VCL在体内和体外PCa进展中的作用。研究结果表明了VCL可以成为PCa预后和治疗的潜在靶点。
原始出处:
Xiaonan Zheng, Hang Xu, Lina Gong et al. Vinculin orchestrates prostate cancer progression by regulating tumor cell invasion, migration, and proliferation. Prostate. Mar 2021
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#迁移#
36
#肿瘤细胞#
50
#ROS#
34
#PRO#
37
前列腺癌相关研究,学习了,谢谢梅斯
58