中国首部PD-1/PD-L1单抗使用后导致的肺炎诊疗共识重磅发布!:2019 CTS
2019-09-08 小M MedSci原创
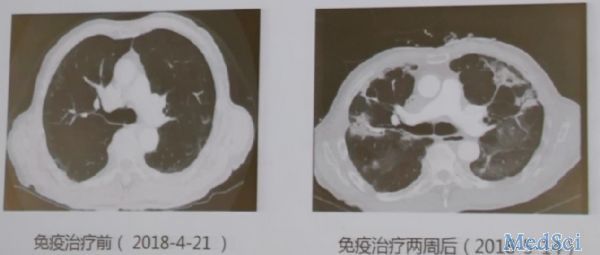
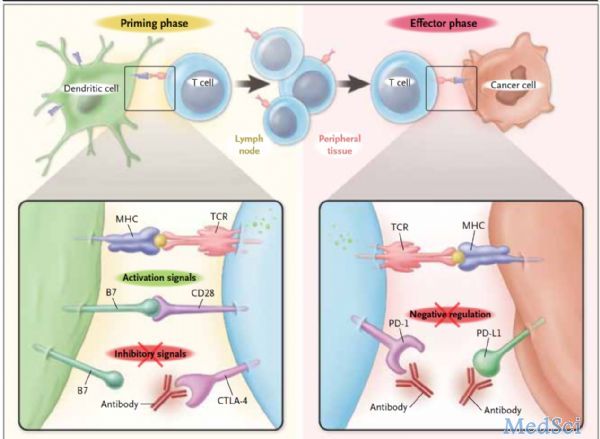
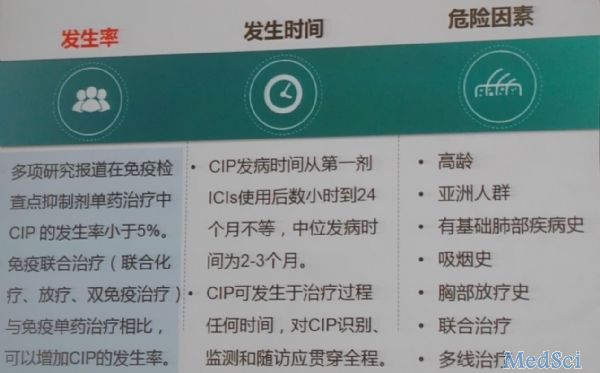
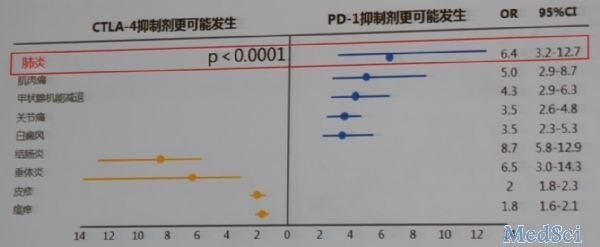
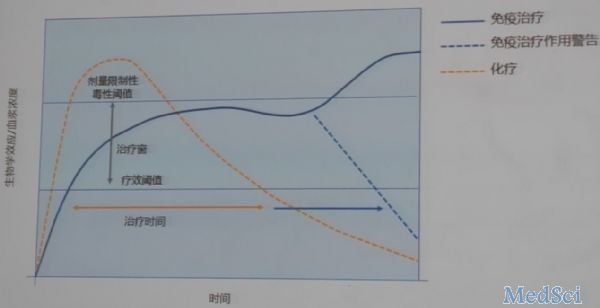
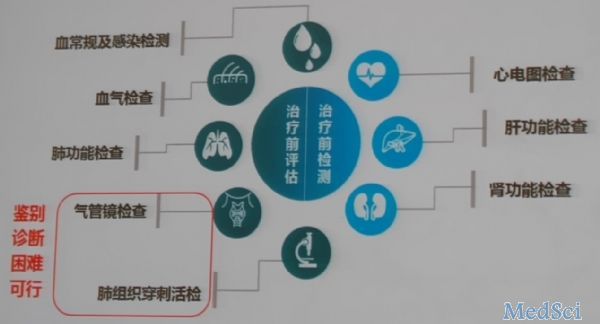
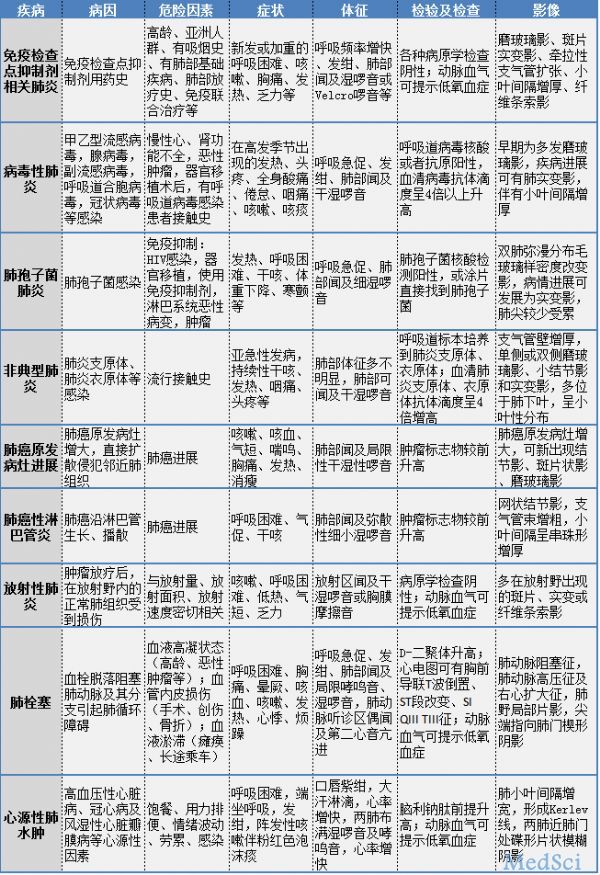
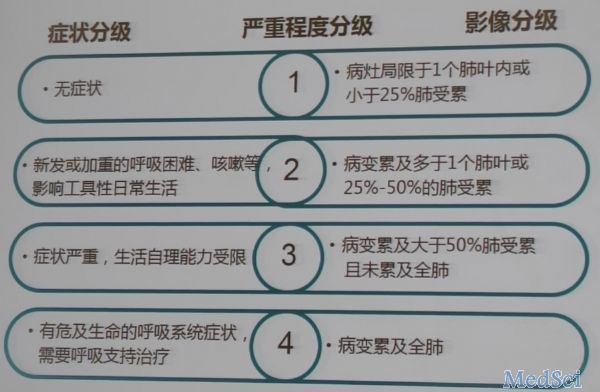
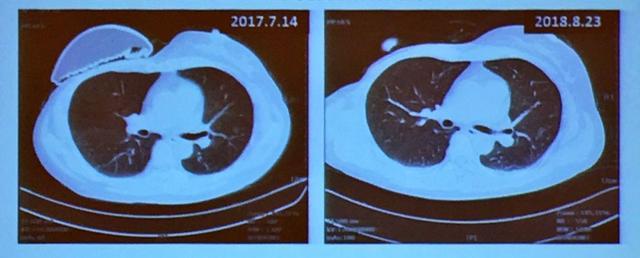
中国首部PD-1/PD-L1单抗使用后导致的肺炎诊疗共识发布肺癌免疫治疗是继手术、放化疗后新兴的肿瘤治疗手段。免疫检查点抑制剂(ICIs)被认为是迄今为止最成功的肿瘤免疫疗法,在非小细胞肺癌治疗中表现出良好疗效。但有些患者使用ICIs后会出现免疫检查点抑制剂相关肺炎(CIP),临床发生率低,但易造成免疫治疗延迟或终止,严重可导致死亡。由于免疫抑制剂的兴起,为了更好地帮助临床医生能更好地应对CI
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言
















👍
40
#PD-L1#
43
#CTS#
38
#PD-L1单抗#
30
#重磅#
43
学习了
69