NEJM:Sotrovimab可降低新冠肺炎高风险人群病情进展风险
2021-10-28 MedSci原创 MedSci原创
研究认为,在接受Sotrovimab治疗后,病程早期但存在病情进展高风险因素的新冠肺炎患者不良预后风险显著降低,且安全性良好

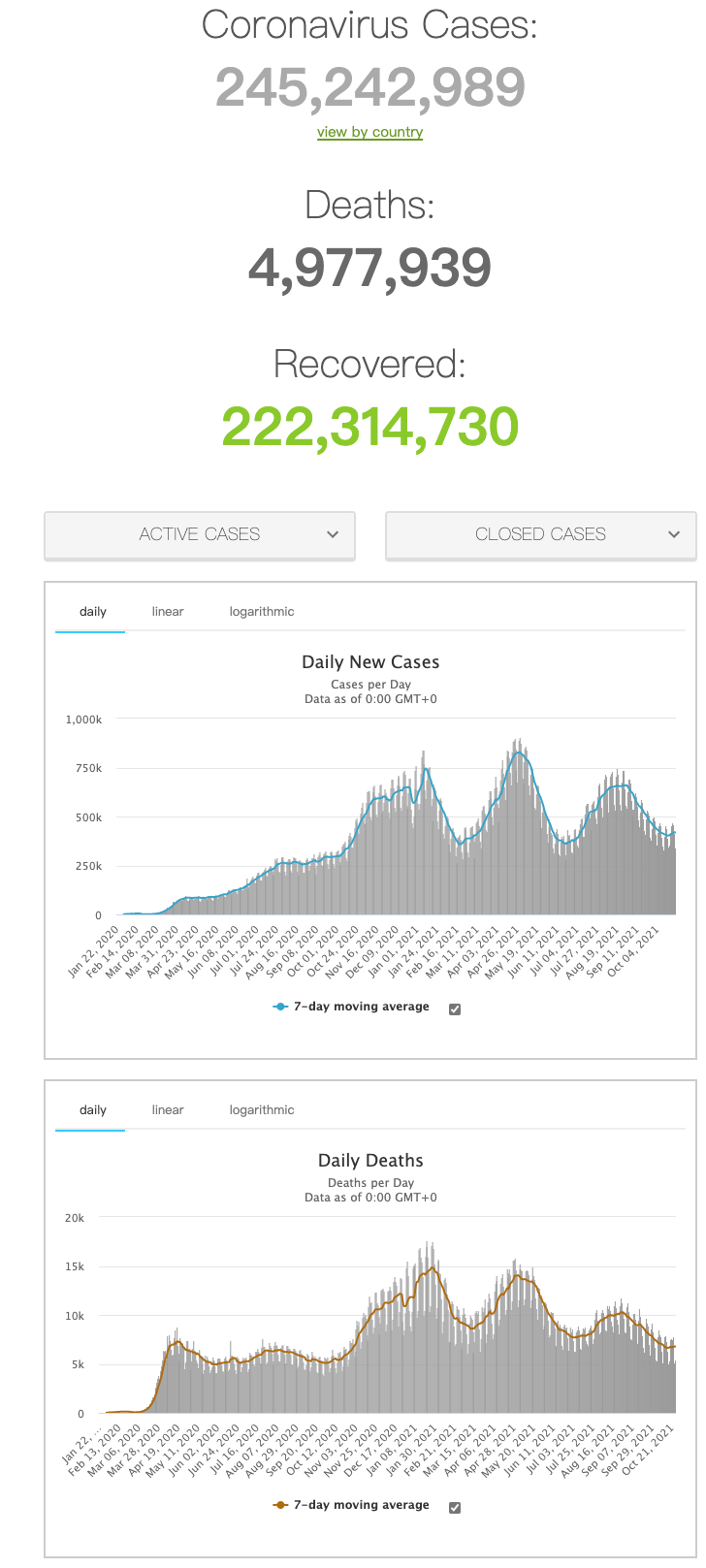
新冠肺炎的全球大流行已导致超过480万人死亡。仅在美国,截至2020年秋季,已有96-240万例Covid-19相关住院病例,在2021年1月,79%的ICU病床被新冠肺炎患者占用。老年以及并发肥胖、糖尿病、慢性阻塞性肺疾病和慢性肾脏疾病的患者是新冠肺炎住院或死亡的高风险人群,预防高危患者病情进展对新冠肺炎的治疗至关重要。Sotrovimab是一种泛Sarbe冠状病毒亚属单克隆抗体,旨在防止病程早期高危患者Covid-19的进展,近日研究人员公布了Sotrovimab的III期临床研究结论。
这项多中心、双盲、III期试验中,有症状的Covid-19 (症状出现到治疗的时间少于5天)并伴有至少一个疾病进展风险因素的非住院患者参与,随机接受单次输注剂量500 mg的Sotrovimab或安慰剂。研究的主要疗效结果是随机分组后29天内因任何原因住院治疗(24小时以上)或死亡。
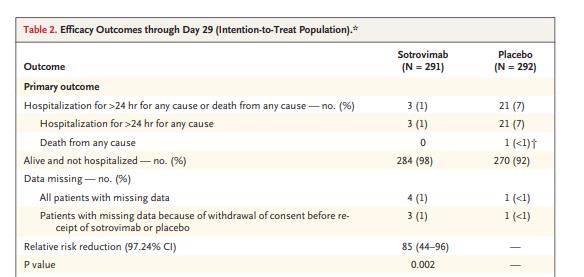
本次研究为中期分析结论,疗效终点评估包括583名患者,其中Sotrovimab组291名,安慰剂组292名。Sotrovimab组3名患者(1%)因疾病进展导致住院或死亡,而安慰剂组高达21名患者(7%),Sotrovimab治疗使患者病情进展的相对风险降低了85%。安慰剂组有5名患者入住重症监护病房,其中1名患者在第29天死亡。868名患者接受了安全性评估,其中Sotrovimab组430名,安慰剂组438名,Sotrovimab组17%的患者报告了不良事件,而安慰剂组不良事件率为19%。Sotrovimab组的严重不良事件发生率低于安慰剂组(2% vs 6%)。
Sotrovimab治疗后患者不良预后风险降低
研究认为,在接受Sotrovimab治疗后,病程早期但存在病情进展高风险因素的新冠肺炎患者不良预后风险显著降低,且安全性良好。
原始出处:
Anil Gupta et al. Early Treatment for Covid-19 with SARS-CoV-2 Neutralizing Antibody Sotrovimab. N Engl J Med,October 27,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#mAb#
25
#高风险#
35
#病情#
35
#OTR#
27
学习了
70