EBCC-11︱乳腺癌寡转移的局部治疗
2018-04-07 徐莹莹 金锋 肿瘤瞭望
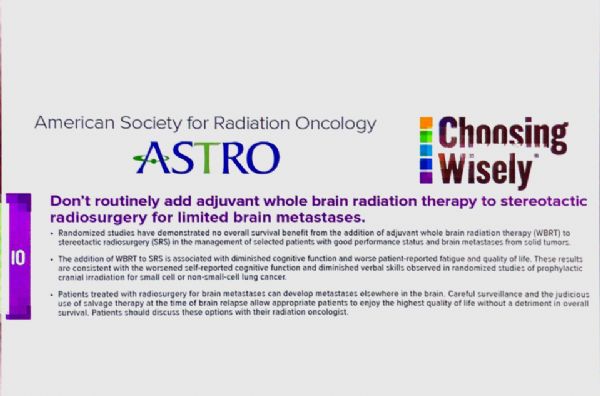
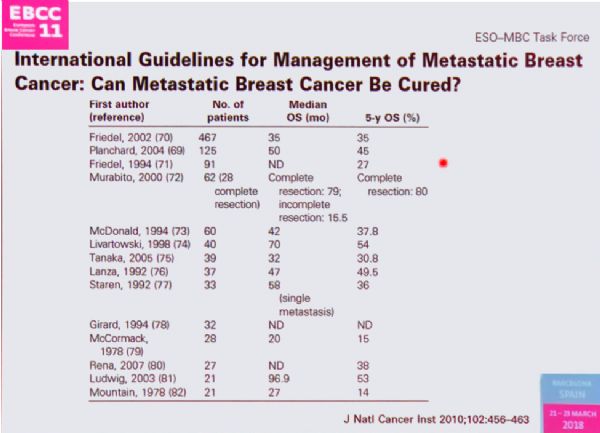
2018年3月21日,第11届欧洲乳腺癌大会(EBCC-11)于西班牙巴塞罗那举行。会议第二天上午,来自荷兰、意大利等国家的讲者分别对乳腺癌寡转移病灶的生物学特性、局部治疗价值、颅内外寡转移灶的局部处理方式进行了系统梳理,现将报告精要整理如下。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











学习了.谢谢作者分享!
136
#局部#
49
#局部治疗#
37
学习了
129
学习
134