Spine:术前冠状位脊柱不平衡对术后功能无显著影响
2013-05-29 Spine dxy
脊柱畸形矫正时恢复脊柱冠状位和矢状位的平衡一直是脊柱外科医生工作的主要目标。从术后X片的角度来说,大部分患者均能达到矢状位和冠状位矫形的平衡,但其最终的临床功能预后确并不一定好,对脊柱外科医生而言,如何达到完美矫正畸形目的的同时改善患者的功能预后一直是一个挑战。既往已有对矫形术后影像学X片和矫形功能预后相关性进行的研究,矢状位不平衡会对患者术后产生不利影响,如疼痛增加,功能预后变差等,该结论不前已
脊柱畸形矫正时恢复脊柱冠状位和矢状位的平衡一直是脊柱外科医生工作的主要目标。从术后X片的角度来说,大部分患者均能达到矢状位和冠状位矫形的平衡,但其最终的临床功能预后确并不一定好,对脊柱外科医生而言,如何达到完美矫正畸形目的的同时改善患者的功能预后一直是一个挑战。既往已有对矫形术后影像学X片和矫形功能预后相关性进行的研究,矢状位不平衡会对患者术后产生不利影响,如疼痛增加,功能预后变差等,该结论不前已经得到统一的认识,但关于冠状位不平衡但研究结果不一,有学者认为,冠状位脊柱排列不平衡和患者的疼痛评分并无相关性,而有些学者认为,冠状位不平衡(>4cm)可以显著影响脊柱畸形矫形术后患者的SRS-22和ODI功能评分。近日来自韩国首尔Wooridul脊柱中心的医生就术前脊柱畸形冠状位不平衡对术后功能效果的影响进行了较大样本的研究,相关结论发表在spine杂志上。
共85例(73女,12男)脊柱畸形患者纳入本研究,平均年龄56岁,平均随访时间49月,所有患者均接受手术治疗矫正脊柱畸形,51例后路,34例前后路联合,1例单纯前路。上述患者的脊柱冠状位不平衡均>4cm,年龄均大于20岁,术后至少随访2年,并且术前,术后存在完整的影像学和功能评估随访资料。
将上述患者按照是否合并脊柱矢状位不平衡分为两组:甲组,23例,患者冠状位不平衡>4cm,不伴有矢状位不平衡>5cm;乙组,62例,患者冠状位不平衡>4cm,合并矢状位不平衡>5cm.对两组患者,比较基本人口统计学数据,术后胸椎,胸腰椎,腰椎Cobb角,冠状位平衡,矢状位平衡,ODI,SRS功能评分等指标。
研究结果提示:共85%(72/85)的患者术后的冠状位平衡得到改善,13例患者的C7垂直线距离超过10mm,胸椎术前平均Cobb角34度,术后纠正为22度;胸腰椎术前平均Cobb角44度,术后纠正为30度。
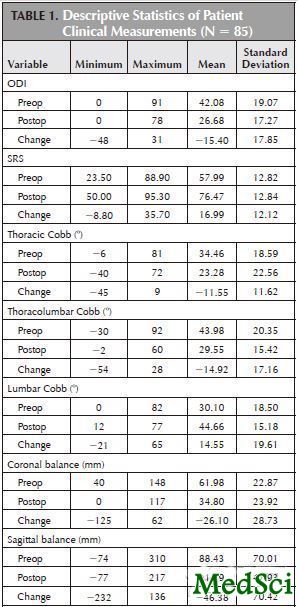
患者术后功能等各项指标较术前均有显著改善,如表1所示。
表1:患者总体统计数据比较
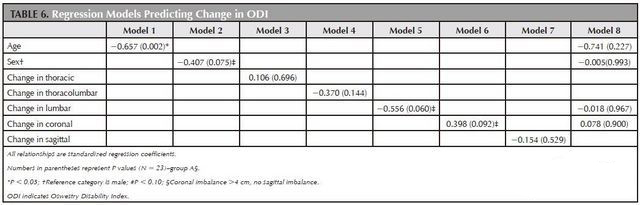
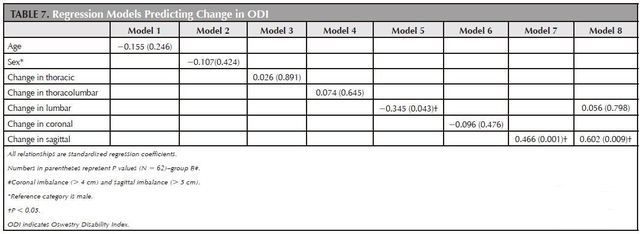
对和ODI指标相关的数据进行线性回归模型分析,发现年龄,腰椎Cobb角改变,矢状位平衡3个因素和ODI(n=85)改变有显著相关性,但对年龄和腰椎Cobb角进行变量控制后仍可发现矢状位不平衡和ODI评分相关(model1-7分别对应:年龄,性别,胸椎Cobb角改变,胸腰椎Cobb角改变,腰椎Cobb角改变,冠状位不平衡,矢状位不平衡,Model 为对年龄和腰椎Cobb角改变进行变量控制后矢状位平衡对ODI计分的影响),结果如表2所示。
表2:以ODI作为变量的线性回归分析结果
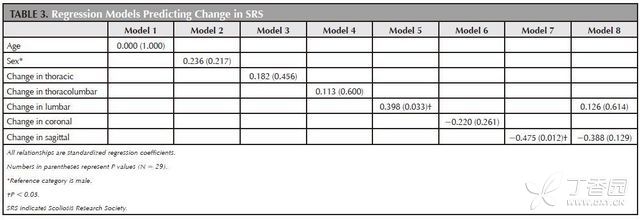
对和SRS(n=29)指标相关的数据进行线性回归模型分析,发现腰椎Cobb角改变和矢状位不平衡对SRS有显著影响,如表3所示。
表3:以SRS作为变量的线性回归分析结果
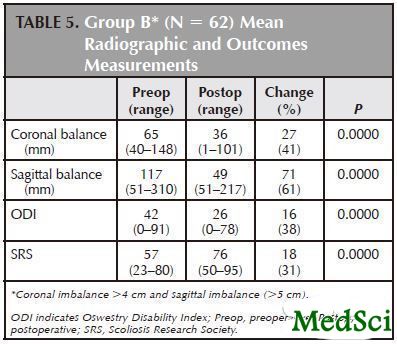
甲组的相关统计学指标如表4所示,ODI平均改善33%,SRS平均改善22%;乙组统计学指标如表5所示,冠状位不平衡平均改善41%,矢状位不平衡平均改善61%,ODI平均改善38%,SRS平均改善31%,组间主要指标比较,如术后矢状位平衡,术前术后ODI、SRS,ODI、SRS数值改善程度等均无显著差异。
表4:甲组患者相关数据统计学指标
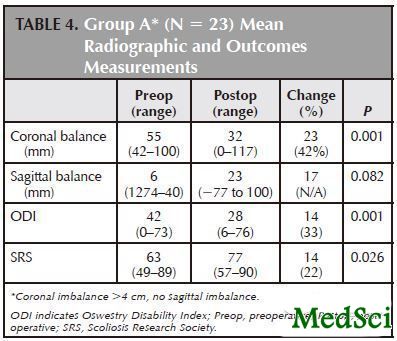
表5:乙组患者相关数据统计学指标
甲组患者对和ODI指标相关的数据进行线性回归模型分析,发现年龄是ODI变化的唯一显著相关因素,如表6所示;乙组患者对和ODI指标相关的数据进行线性回归模型分析,发现腰椎Cobb角和矢状位不平衡改变是ODI变化的显著相关因素,如表7所示.。
表6:甲组患者以ODI作为变量的线性回归分析结果
表7:乙组患者以ODI作为变量的线性回归分析结果
据上述研究结果,作者总结:矢状位平衡改善是患者术后功能评分恢复良好的最佳预测因子,冠状位脊柱不平衡的改善对患者最终的功能预后无显著影响。

Does correction of preoperative coronal imbalance make a difference in outcomes of adult patients with deformity?
STUDY DESIGN
Retrospective study with prospectively collected outcomes data.
OBJECTIVE
Determine the significance of coronal balance on spinal deformity surgery outcomes.
SUMMARY OF BACKGROUND DATA
Sagittal balance has been confirmed as an important radiographic parameter correlating with adult deformity treatment outcomes. The significance of coronal balance on functional outcomes is less clear.
METHODS
Eighty-five patients with more than 4 cm of coronal imbalance who underwent reconstructive spinal surgery were evaluated to determine the significance of coronal balance on functional outcomes as measured with the Oswestry Disability Index (ODI) and Scoliosis Research Society outcomes questionnaires. Sixty-two patients had combined coronal (>4 cm) and sagittal imbalance (>5 cm), while 23 patients had coronal imbalance alone.
RESULTS
Postoperatively, 85% of patients demonstrated improved coronal balance. The mean improvement in the coronal C7 plumb line was 26 mm for a mean correction of 42%. The mean preoperative sagittal C7 plumb line in patients with combined coronal and sagittal imbalance was 118 mm (range, 50-310 mm) and improved to a mean 49 mm. The mean preoperative and postoperative ODI scores were 42 (range, 0-90) and 27 (range, 0-78), for a mean improvement of 15 (36%) (P = 0.00001; 95% CI, 12-20). The mean Scoliosis Research Society scores improved by 17 points (29%) (P = 0.00). Younger age (P = 0.008) and improvement in sagittal balance (P = 0.014) were positive predictors for improved ODI scores. Improvement in sagittal balance (P = 0.010) was a positive predictor for improved Scoliosis Research Society scores. In patients with combined coronal and sagittal imbalance, improvement in sagittal balance was the most significant predictor for improved ODI scores (P = 0.009). In patients with preoperative coronal imbalance alone, improvement in coronal balance trended toward, but was not a significant predictor for improved ODI (P = 0.092).
CONCLUSION
Sagittal balance improvement is the strongest predictor of improved outcomes in patients with combined coronal and sagittal imbalance. In patients with coronal imbalance alone, improvement in coronal balance was not a factor for predicting improved functional outcomes.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#Spine#
33