Spine:融合至骶骨可改善脊柱畸形矫形术后长期效果
2014-06-25 orthowhq 丁香园
矫正成人僵硬型脊柱畸形,即使对最有经验的脊柱外科医师而言,极富挑战性。一个重要的考虑因素为远端融合止点,即需决定止于腰椎还是骶骨。尽管有绝大多数一致的适应症,固定止于骶骨,但此结论常靠手术医师的意愿和经验。 保留腰椎的活动节段可减少近端胸腰段融合处的应力,降低假关节的发生,但可能导致融合节段远端症状性退变,而需再手术将融合节段延伸至骶骨。 长节段融合止于腰椎,除保留一定的运动功能外
矫正成人僵硬型脊柱畸形,即使对最有经验的脊柱外科医师而言,极富挑战性。一个重要的考虑因素为远端融合止点,即需决定止于腰椎还是骶骨。尽管有绝大多数一致的适应症,固定止于骶骨,但此结论常靠手术医师的意愿和经验。
保留腰椎的活动节段可减少近端胸腰段融合处的应力,降低假关节的发生,但可能导致融合节段远端症状性退变,而需再手术将融合节段延伸至骶骨。
长节段融合止于腰椎,除保留一定的运动功能外,手术范围小,植骨量相对少,融合节段相对少。但必须考虑远端邻近节段退变的可能,长节段融合远端影像学上崩塌,发生率为16%到67%,为12%到14%最终将融合节段延伸至骶骨。目前关于融合节段延伸至骶骨的长期放射和临床疗效,尚未见报道。
美国华盛顿大学骨科的学者进行了一项前瞻性数据库的回顾性研究,提示脊柱畸形术后将融合节段延伸至骶骨的长期疗效明显,文章于2014年5月发表在Spine上。
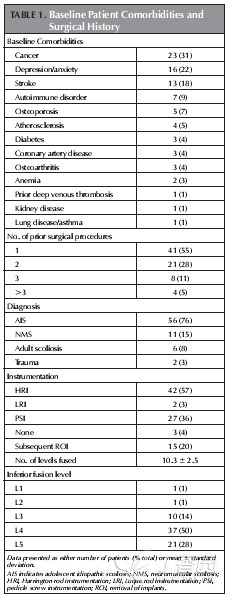
该研究共纳入了作者所在单中心,74例行长节段融合(5个节段以上,近端融合于胸椎)后又将融合节段延伸至骶骨的病例(表1),评估指标包括Oswestry残障指数,SRS分数和/或影像学参数,时间点为术前基准,术后6周,1年,2年,3年和/或5年,记录并发症情况。
表1 术前病例一般情况和手术史。其中可见,青少年特发性脊柱侧弯为原融合手术最常见的指证,Harrington棒最常见,平均融合节段为11个,L4为最常见的远端止点。。
病例的平均年龄49岁(19-76岁),平均随访时间4.5年(3月-10年)。所有病例起初融合节段远端节段退变,72%(53例)存在矢状位固定的不平衡。
研究结果显示,Oswestry残障指数和SRS分数均改善,且随访5年无加重(图1)。与术前基准(平均78mm)相比,术后任何时间点的矢状序列(SVA)均得到改善,但第1年至第5年加重(平均21mm到44mm)(图2)。30%病例(22例)发生了重要并发症,15例(20%)进行了17次翻修手术。有并发症和翻修手术的病例,5年随访时,临床疗效评估与无并发症和未翻修的病例类似。
以上结果表明,将长融合节段延长至骶骨,经5年的随访,临床疗效和脊柱序列均有明显改善。尽管30%的病例发生了重要并发症,20%的病例翻修,但疗效评估与其它病例类似。重要并发症中,3个月以内主要是运动神经根病,3个月以后主要是假关节形成。翻修的主要原因为假关节,其次为术后神经根性病,交界区失败,深部感染。本研究首次阐明了延长长节段融合至骶骨的临床疗效,尽管并发症发生率相对较高,但并不影响临床疗效。并发症发生的危险因素,有待进一步研究。
原始出处:
OʼNeill KR, Bridwell KH, Lenke LG, Chuntarapas T, Dorward I, Neuman B, Ahmad A, Baldus C.Extension of spine fusion to the sacrum following long fusions for deformity correction.Spine (Phila Pa 1976). 2014 May 20;39(12):953-62
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#长期效果#
32
#Spine#
28
#畸形#
24
#脊柱畸形#
0
#融合#
35