Eur Heart J-Card Img:主动脉狭窄患者检测心脏淀粉样变的超声心动图指标
2022-08-14 MedSci原创 MedSci原创
基于超声心动图检查的参数在检测AS患者CA方面有很大的前景。进一步的研究应该探索这些超声心动图变量的最佳临界值,以获得更好的诊断准确性。
主动脉瓣狭窄(Aorticstenosis,AS)和心脏淀粉样变(Cardiacamyloidosis,CA)常常同时存在,但在AS患者中CA的诊断仍然是一个挑战。
近日,心血管领域权威杂志Eur Heart J-Card Img上发表了一篇研究文章,研究人员的目的是评估超声心动图参数,这可能有助于在AS患者中检测有无CA。
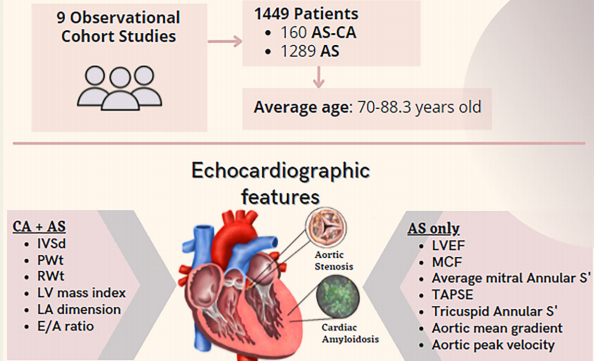
研究人员对电子数据库中的同行评议文献进行了系统的文献检索,检索时间从数据库成立到2022年1月10日。在纳入的1449例患者中,160例患者同时患有AS和CA,而剩下的1289例患者仅患有AS。
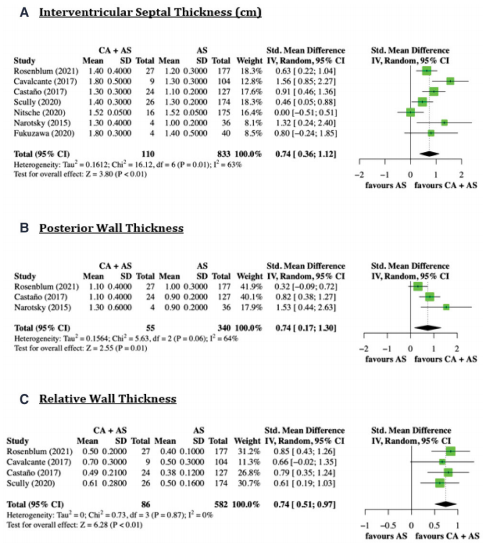
研究人员通过Meta分析,结果显示室间隔厚度[标准化均数差值为0.74,95%CI为0.36-1.12,P=0.0001)、相对壁厚(标准化均数差值为0.74,95%CI为0.17-1.30,P<0.0001)、后壁厚度(标准化均数差值为0.74,95%CI为0.51-0.97,P=0.0011)、左室质量指数(标准化均数差值为1.62,95%CI为0.63-2.62,P=0.0014)、E/A比值(标准化均数差值为4.18,95%CI为1.91-6.46,P=0.0003)和LA维度(标准化均数差值为0.73,95%CI为0.43-1.02,P<0.0001)]在同时患有AS和CA的患者中显著高于单纯AS患者。与此相反,同时患有AS和CA患者的心肌收缩分数(标准化均数差值为−2.88,95%CI为−5.70~−0.06,P=0.045)、平均二尖瓣环S′(标准化均数差值为−1.14,95%CI为−1.86~−0.43,P=0.0017)、三尖瓣环平面收缩幅度(标准化均数差值为−0.36,95%CI为−0.62~−0.09,P=0.0081)和三尖瓣环S′(标准化均数差值为−0.77,95%CI为−1.13~−0.42,P<0.0001)显著降低。
由此可见,基于超声心动图检查的参数在检测AS患者CA方面有很大的前景。进一步的研究应该探索这些超声心动图变量的最佳临界值,以获得更好的诊断准确性。
原始出处:
Vikash Jaiswal.et al.Echocardiographic predictors of presence of cardiac amyloidosis in aortic stenosis.Eur Heart J-Card Img. 2022.https://academic.oup.com/ehjcimaging/advance-article/doi/10.1093/ehjci/jeac146/6655774
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#心脏淀粉样变#
46
#心动图#
48
#主动脉狭窄#
35
#ART#
41
#淀粉样变#
45
#主动脉#
47
#动脉狭窄#
37
#HEART#
34