J Clin Oncol:乐伐替尼联合经动脉化疗栓塞可显著改善晚期肝癌患者预后
2022-08-05 MedSci原创 MedSci原创
乐伐替尼加用经动脉化疗栓塞可改善晚期肝细胞癌患者的临床预后
乐伐替尼(LEN)是晚期肝细胞癌(HCC)患者的一线治疗药物;然而,它显示出适度的生存益处。该研究旨在比较 LEN 联合经动脉化疗栓塞 (LEN-TACE) 与 LEN 单药治疗晚期 HCC 患者的临床预后。
这是一项在我国开展的多中心、随机、开放标签、平行组、III期试验,初次治疗或手术后初次复发的晚期 HCC 患者被随机 (1:1) 分组接受 LEN 联合按需 TACE (LEN-TACE) 或 LEN 单药治疗。在随机分组后3天内开始予以 LEN(初始剂量:体重≥60 kg,12 mg/日;体重<60 kg,8 mg/日)。TACE 在 LEN 开始一天后启动。主要终点是总生存期(OS)。
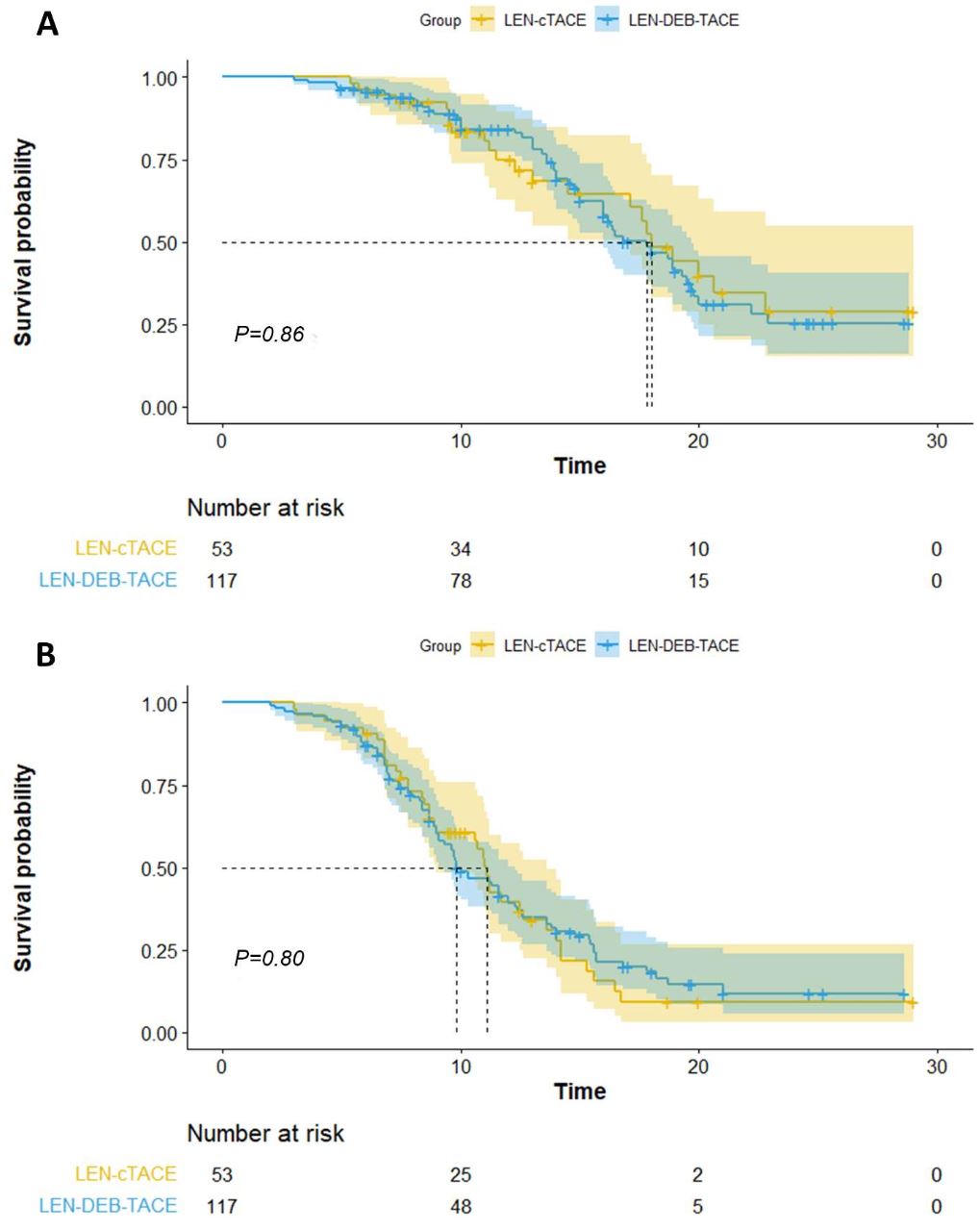
两组患者的总生存率和无进展生存率
2019年6月-2021年7月,共338位患者被随机分至两组:LEN-TACE 组 170位,LEN 组 168位。中位随访了17.0个月后,LEN-TACE组的中位总生存期显著长于 LEN 组(17.8 vs 11.5个月;HR 0.45,p<0.001)。LEN-TACE组和 LEN 组的中位无进展生存期分别是10.6个月和6.4个月(HR 0.43,p<0.001)。LEN-TACE 组的患者有更高的客观缓解率(54.1% vs 25.0%,p<0.001)。多变量分析显示,门静脉癌栓和治疗分配是 OS 的独立危险因素。
综上,乐伐替尼加用经动脉化疗栓塞可改善晚期肝细胞癌患者的临床预后,或可成为这类患者的潜在一线治疗方案。
原始出处:
Zhenwei Peng, et al. Lenvatinib Combined With Transarterial Chemoembolization as First-Line Treatment for Advanced Hepatocellular Carcinoma: A Phase III, Randomized Clinical Trial (LAUNCH). Journal of Clinical Oncology. https://ascopubs.org/doi/abs/10.1200/JCO.22.00392
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#化疗栓塞#
43
#肝癌患者#
34
#Oncol#
35
#患者预后#
51