Allergy:过敏性鼻炎中CD23的表达建立T-B细胞互作
2020-04-17 AlexYang MedSci原创
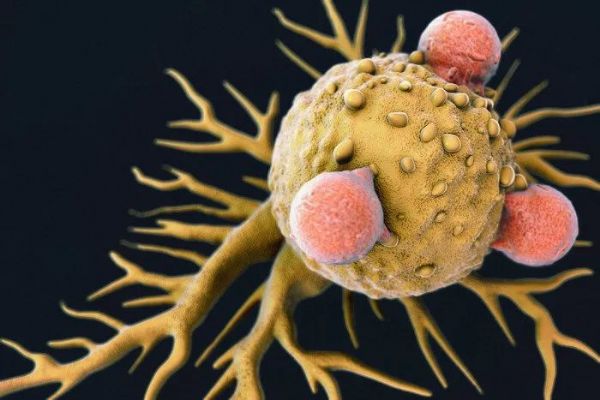
B细胞亚群和T-B细胞互作对过敏性鼻炎的贡献以及过敏原免疫治疗(AIT)的机制仍旧了解甚少。最近,有研究人员在AR患者中探究了循环B细胞特征、潜在机制和与AIT临床响应相关性。
B细胞亚群和T-B细胞互作对过敏性鼻炎的贡献以及过敏原免疫治疗(AIT)的机制仍旧了解甚少。最近,有研究人员在AR患者中探究了循环B细胞特征、潜在机制和与AIT临床响应相关性。
研究发现,在AR患者中,循环记忆B细胞的频率和绝对数量增加;CD23在CD19+ CD20+ CD27+ IgD-开关记忆B细胞中的表达显著增强,并且与抗原特异性lgE水平、症状得分和Tfh2/Tf细胞比例有关。与健康对照相比,AR患者的Tfh2细胞通过IL-4诱导开关记忆B细胞CD23表达的能力更强,并且不能被AR相关的具有IL-10表达缺陷的Tfr细胞充分抑制。在12个月的AIT治疗后,AR患者中开关记忆B细胞的CD23表达下调,且与疾病减轻正相关。
最后,研究人员指出,在AR患者中,CD23表达搭建的T-B细胞互作参与了疾病病理和AIT机制。
原始出处:
Yao Y, Wang N, Chen CL et al. CD23 expression on switched memory B cells bridges T-B cell interaction in allergic rhinitis. Allergy. 21 Mar 2020.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#过敏性#
26
#B细胞#
19
#ALL#
0
#互作#
27
好
97
论文期刊联系V(jiaowobabb)
76