Sci Transl Med:癌症手术中照一照即可检出转移的前哨淋巴结?
2021-05-08 MedSci原创 MedSci原创
癌症约影响了全球三分之一的人口。手术仍是局限性癌症的主要治愈方法,但良好的预后需要彻底切除原发肿瘤和及时发现转移灶。
癌症约影响了全球三分之一的人口。手术仍是局限性癌症的主要治愈方法,但良好的预后需要彻底切除原发肿瘤和及时发现转移灶。
为了扩展手术能力并改善患者预后,Blair等研究人员开发了一种六通道彩色/近红外图像传感器,其灵感来自螳螂虾视觉系统,该系统在手术过程中可指导近红外荧光图像。
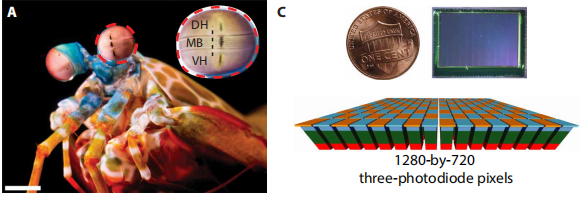
螳螂虾的眼睛和生物启发图像传感器
螳螂虾独特的眼睛,可最大程度地增加贡献给它的光子数量以及周围每一次瞥见所包含的信息量。Blair等人在其单芯片系统中模拟了螳螂虾的视觉特点,该芯片系统集成了垂直堆叠的硅光电探测器和像素化光谱滤光片的阵列。
图像传感器的成像能力
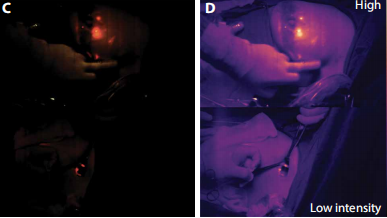
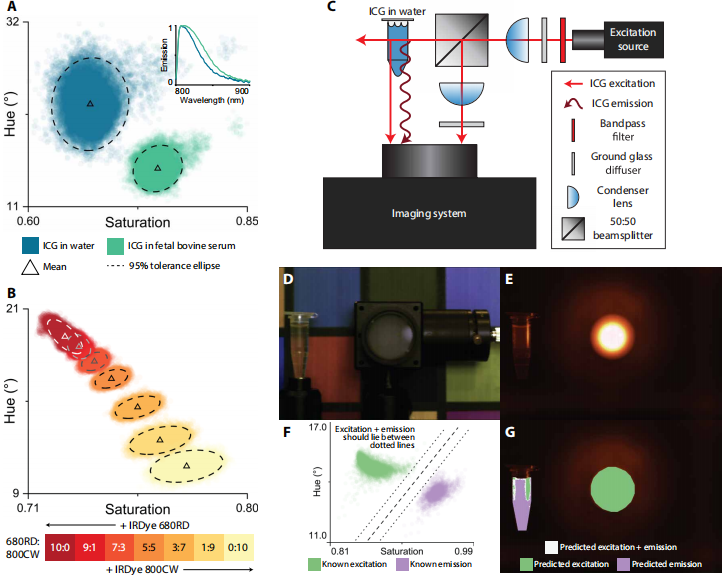
为了提供单个仪器无法提供的有关肿瘤位置的信息,研究人员调整了三个颜色通道,以直观地观察手术过程,并调整了三个近红外通道,以对突出探针癌组织的光学探头进行多功能成像。
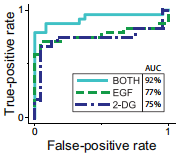
不同方法的肿瘤检出率
在移植了人前列腺肿瘤的无胸腺小鼠中,该图像传感器可同时检测两种靶向肿瘤的荧光团,从而约可区分92%的病例中的肿瘤病灶与健康组织。此外,其还允许提取近红外结果图示,从而将肿瘤和手术部位的三维形态映射出来,而且误差保持在1.2mm范围内。
乳腺癌手术中检出前哨淋巴结
在手术室中,对18例乳腺癌患者进行手术切除期间,该图像传感器使用临床认可的近红外荧光团进一步实现了前哨淋巴结的定位。
综上所述,这种简单而小巧的架构所提供的灵活性和性能,突出了受生物启发而来的传感器在图像引导手术中的优势。
原始出处:
Steven Blair, et al. Hexachromatic bioinspired camera for image-guided cancer surgery. Science Translational Medicine 05 May 2021: Vol. 13, Issue 592, eaaw7067. DOI: 10.1126/scitranslmed.aaw7067
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#TRA#
36
#Transl#
35
写的很棒啊
58
#淋巴结#
24
#前哨淋巴结#
0
#Med#
30