Thyroid:甲状腺功能对止血、凝血和纤溶系统的影响
2021-10-22 从医路漫漫 MedSci原创
未经治疗的甲状腺功能减退症与获得性血管性血友病综合征相关,甲状腺功能亢进症与血栓形成风险增加有关。然而,甲状腺功能对止血、凝血和纤溶的因果影响尚不清楚。
背景:未经治疗的甲状腺功能减退症与获得性血管性血友病综合征相关,甲状腺功能亢进症与血栓形成风险增加有关。然而,甲状腺功能对止血、凝血和纤溶的因果影响尚不清楚。
方法:在一项具有全基因组关联变异的两样本孟德尔随机化(MR)研究中,我们评估了遗传预测的甲状腺功能减退(N=134,641)、正常范围的促甲状腺激素(TSH;N=54,288)和游离甲状腺素(fT4) (N=49,269),甲状腺功能亢进(N=51,823)和甲状腺过氧化物酶抗体阳性(N=25,821)。纤溶酶原激活物抑制剂-1)(N= 2583-120,246)。MR分析以逆方差加权随机效应为主,敏感性分析次之。双侧p<0.05在名义上是显著的,p<0.0011[=0.05/(5个暴露·9个结果)]在主MR分析中为Bonferroni显著。
结果:TSH基因升高与VWF降低相关[β(SE)=-0.020(0.006),p=0.001],与纤维蛋白原降低相关[β(SE)=-0.008(0.002),p=0.001]。遗传上fT4增加与VWF增加相关[β(SE)=0.028(0.011),p=0.012]。基因预测甲状腺功能亢进与VWF增加[β(SE)=0.012(0.004),p=0.006]和FVIII增加[b(SE)=0.013(0.005), p=0.007]相关。基因预测的甲状腺功能减退和甲状腺功能亢进分别与TPA降低[β(SE)=-0.009(0.024),p=0.024]和TPA增加[β(SE)=0.022(0.008),p=0.008]相关。MR灵敏度分析显示方向相似,但精度较低。其他凝血和纤溶因素不确定。

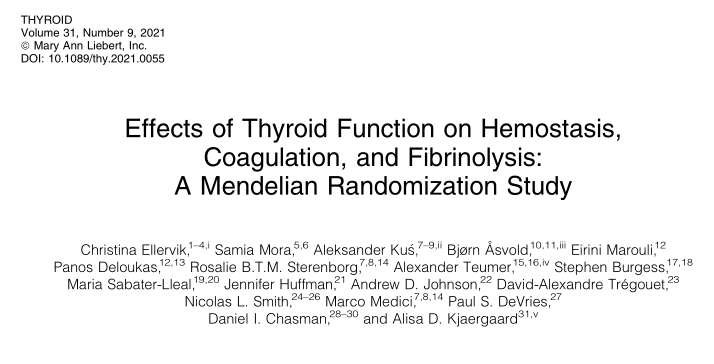
图1 甲状腺功能VWF、FVIII和APTT的孟德尔随机化。结果是基于反方差加权随机效应分析。AITD,自身免疫性甲状腺疾病;b, beta系数;di1 /DIO2,去碘酶1和去碘酶2基因;FVIII VIII因子;SNPs, N,每次分析的单核苷酸多态性数量;TSH、甲状腺刺激激素。
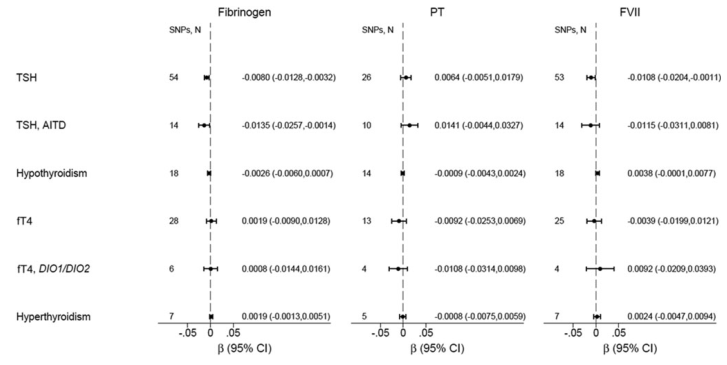
图2 甲状腺功能对纤维蛋白原、PT和FVII的孟德尔随机化。结果是基于反方差加权随机效应分析。fT4游离甲状腺素;FVII第七因子;PT,凝血酶原时间。

图3 D -二聚体、PAI-1(纤溶酶原激活物抑制剂)和组织纤溶酶原激活物(TPA)对甲状腺功能的孟德尔随机化研究结果显示是基于反方差加权随机效应分析。
结论:在目前最大的遗传学研究中,TSH和fT4的基因增加可能分别与VWF合成的减少和增加有关。由于Bonferroni校正可能过于保守,考虑到分析的性状之间的相关性,我们不能否认甲状腺性状与凝血或纤溶因子名义上的关联。
原文出处:
Ellervik C, Mora S, Kuś A,et al.Effects of thyroid function on hemostasis, coagulation, and fibrinolysis: a Mendelian Randomization study.Thyroid 2021 Jul 01
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













学习!有深度
50
#纤溶系统#
42
#止血#
55
谢谢分享
73