Nature:年轻小鼠/人类的脑脊液可以恢复老年小鼠的少突胶质细胞增殖和记忆能力
2022-08-17 brainnew神内神外 brainnew神内神外
年轻人类/小鼠的CSF可以逆转降低的认知功能,这种能力可能是通过OPCs中的Fgf17实现的。这项研究为逆转衰老带来了新的曙光。
最近的研究显示,对生物的系统干预在逆转脑组织的衰老相关方面显示出了巨大的前景,例如转移年轻的血浆到老人的血液中可以使衰老的大脑恢复活力和恢复记忆功能。然而,由于大脑受到血脑屏障的保护,仅仅通过血浆输入可能会限制对这些因素的获取,阻碍它们的年轻化潜力。因此,对于脑细胞的直接环境—脑脊液(CSF)的研究更有必要。
Tony.W教授团队针对该问题,进行了一系列研究,并将其成果“Young CSF restores oligodendrogenesis and memory in aged mice via Fgf17”于2022年5月发表于Nature 杂志。

年轻小鼠/人类CSF
对少突胶质细胞增殖的调控
该团队先对20月龄的老年小鼠进行足部电刺激与光/声音的配对训练,之后将小鼠分为两组,分别注射人工脑脊液(aCSF)和来自年轻小鼠的CSF(YM-CSF)一周,再在训练后的3周进行记忆测试,发现YM-CSF注射组的小鼠具有更好的记忆能力(图1.a,b)。
对小鼠海马进行RNA测序发现,少突胶质细胞相关的基因表达大大上调,且促进少突胶质细胞增殖和分化的转录因子表达也上升(图1.c,d)。此外,海马少突胶质细胞祖细胞(OPC)的增殖和分化也明显增加(图1.e,f),髓鞘形成能力增强(图1.i-k)。
在另一组分别注射年轻人类CSF(YH-CSF)和老年人类CSF(AH-CSF)的小鼠中,也发现注射YH-CSF小鼠的OPC增殖和分化明显增加(图1.g,h),体外OPC培养同样得出该结果,且呈剂量依赖型(图1.l-o)。
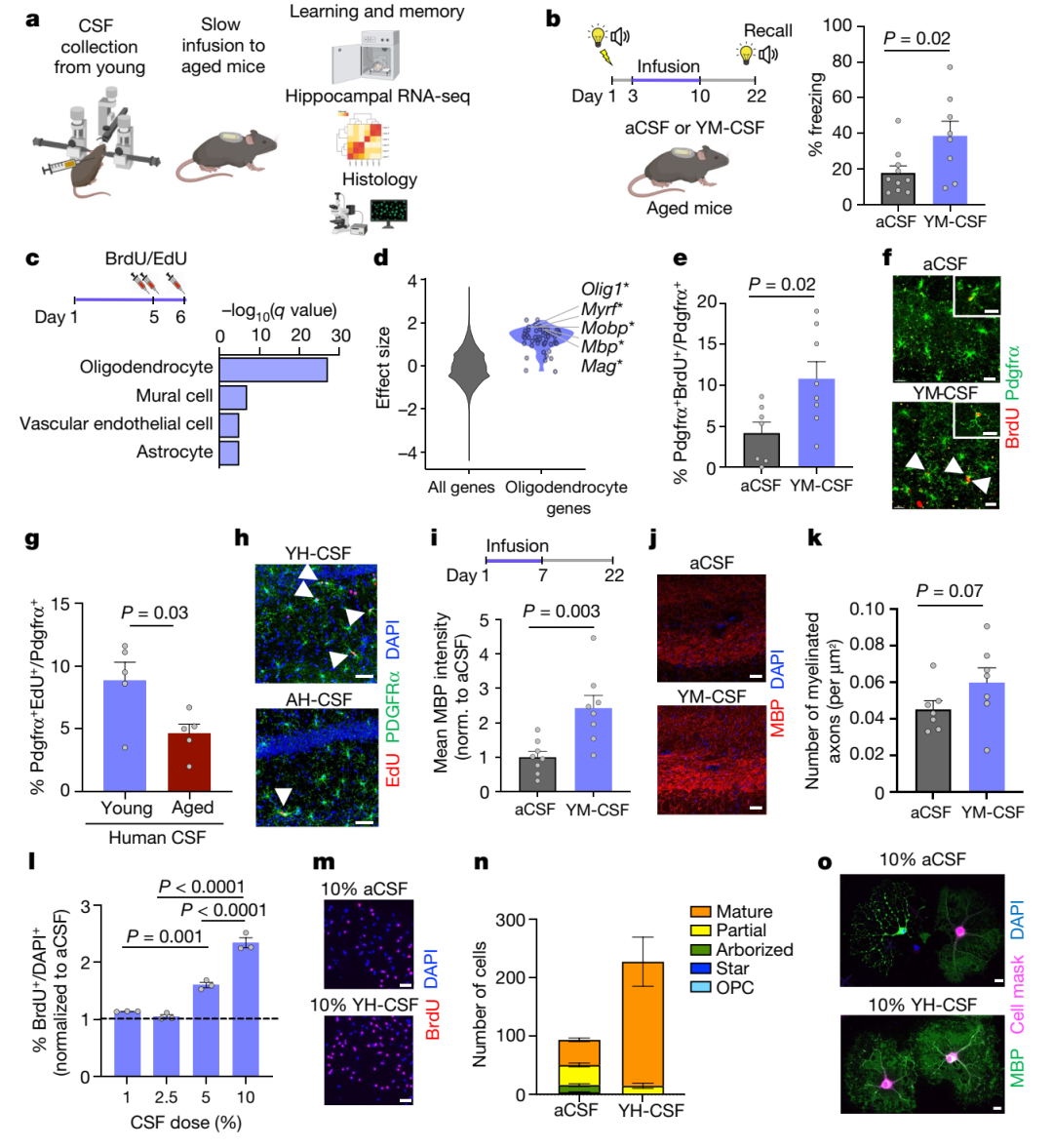 图1. 年轻小鼠/人类的CSF促进了记忆巩固和OPC的增殖和分化
图1. 年轻小鼠/人类的CSF促进了记忆巩固和OPC的增殖和分化
血清应答因子(SRF)介导
年轻小鼠/人类CSF对OPCs的影响
之后该团队用S4 U烷基化RNA代谢测序技术检测暴露于YH-CSF的OPCs,发现暴露1小时后,SRF(通过调控即刻早期基因和肌动蛋白细胞骨架诱导细胞运动、增殖和分化)的基因以及其新生mRNA表达最高,后者在6h之后回到基线,而SRF的靶向基因则在暴露6h后达到最高(图2.a-c)。
此外,YH-CSF暴露6h后的OPCs的肌动蛋白细胞骨架表达也增加(图2.d,e),在YM-CSF注射的小鼠中也得到类似的结果(图2.f,g)。在被敲除SRF的OPCs中重复上述实验,发现敲除SRF之后,YH-CSF对OPCs的效果消失(图2.h-i),说明YH-CSF的效应依赖于SRF。
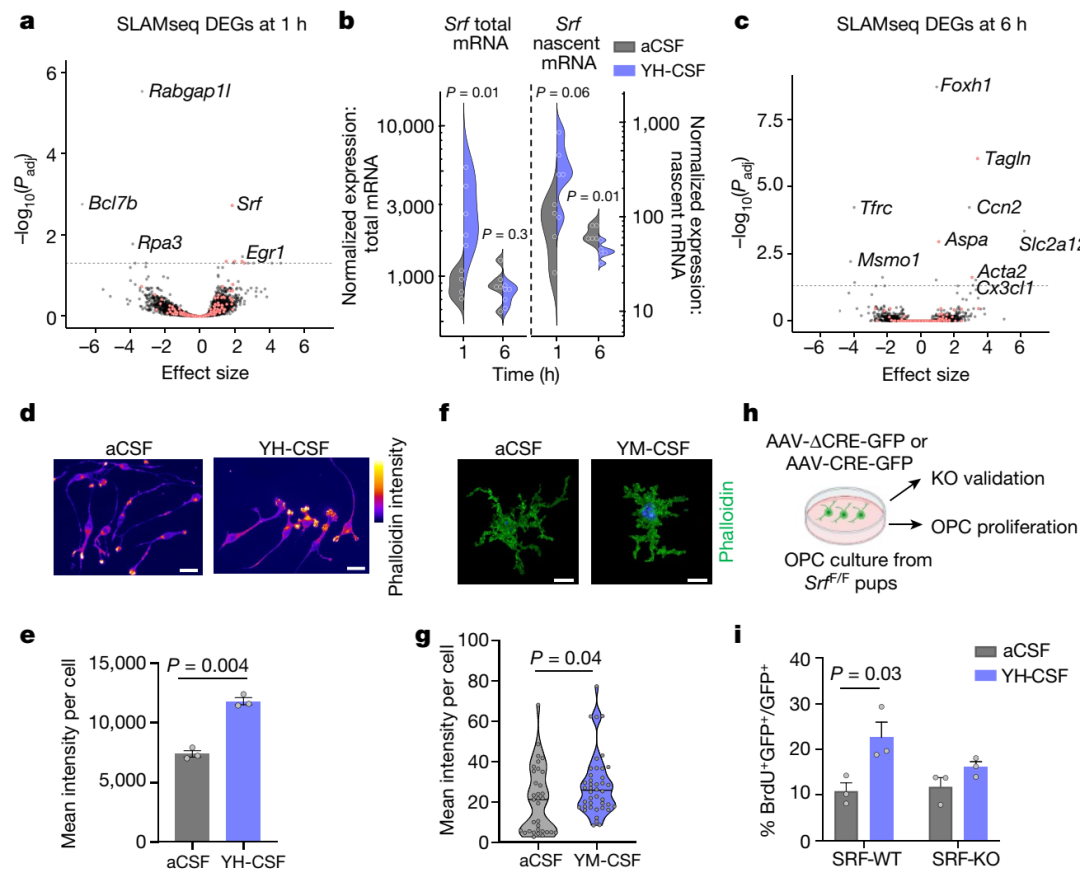
图2.年轻小鼠/人类CSF诱导的SRF可以介导CSF诱导的OPC增殖
在衰老小鼠海马CA1区中也发现,SRF阳性的OPCs数量明显降低(图3.a,b),之后对3月龄小鼠和25月龄小鼠的海马OPCs和成熟少突胶质细胞进行RNA测序,发现OPCs随着衰老,其少突胶质细胞标记物、胶质细胞分化调节、细胞呼吸与代谢以及蛋白质折叠的通路大大被抑制(图3.c,d),且SRF靶向基因的表达也大大降低(图3.e),与其他数据库结果一致(图3.g)。
然而在注射年轻CSF之后,SRF靶向基因的表达会增加,且与GTP酶活性调节、转录因子结合等通路相关(图3.e,f)。
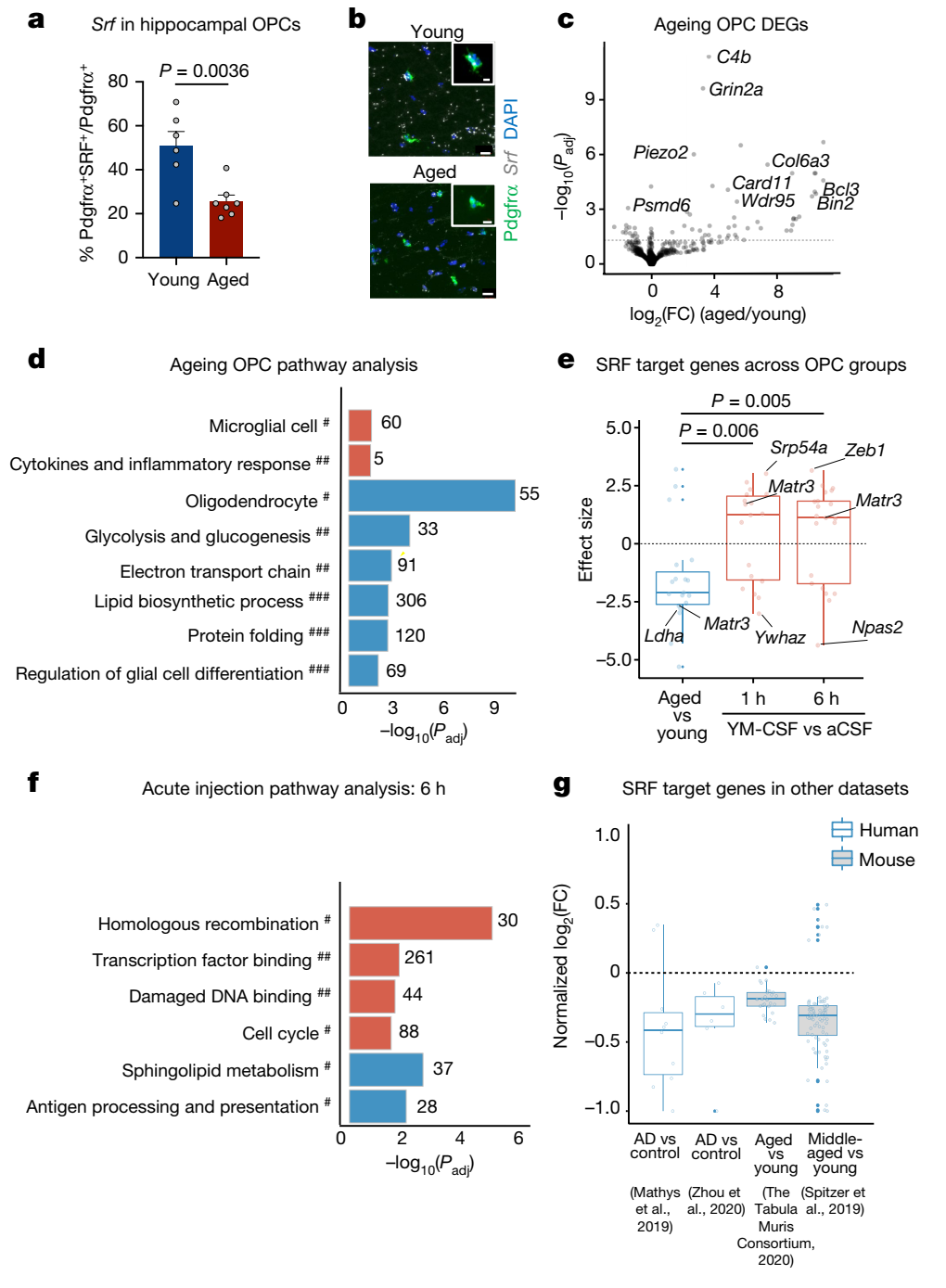
图3. 海马OPCs的SRF信号随着衰老而下调,但能够被年轻小鼠/人类CSF诱导激活
Fgf17可以模拟CSF
对OPCs和记忆的影响
该团队之后在SRE-GFP报告系统的HENK293细胞中对SRF靶向和激活基因进行筛选,发现成纤维细胞生长因子(Fgf)17和Fgf8的效应最强,且呈剂量依赖性(图4.a-d)。由于Fgf17在大脑中富集,因此该团队选择研究Fgf17的作用。研究显示,它的水平在衰老人类的CSF、血液以及小鼠的神经元中降低(图4.e-g),且Fgf17可以通过调节肌动蛋白来激活SRF信号。
之后在体外原代OPCs中,加入Fgf17,发现可以促进OPC增殖和分化(图4.h-k),同时使用上述注射CSF的方法注射重组Fgf17,发现老年小鼠海马中的OPC增殖,且记忆功能改善(图4.l-n)。
之后,在年轻小鼠中注射Fgf17抗体,发现该小鼠的海马依赖的行为学功能下降(Y迷宫,条件恐惧实验),神经可塑性降低(图4.o-r),在体外OPCs中,加入Fgf17抗体也会抑制OPC的增殖(图4.s)。
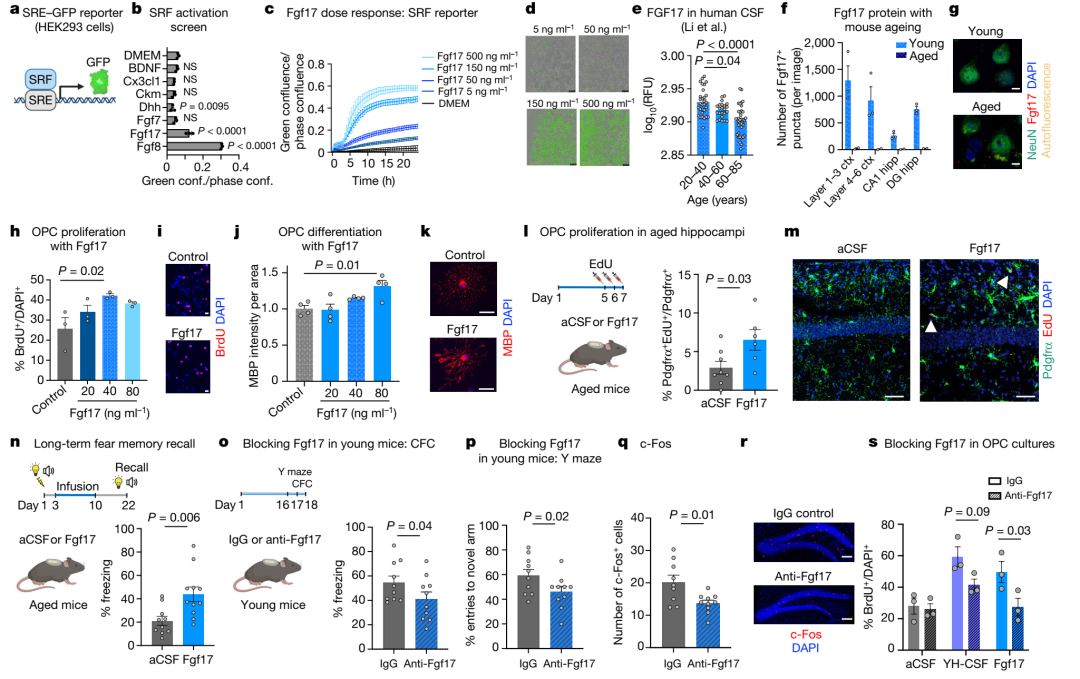
图4. Fgf17 可以促进 OPC 增殖以及改善记忆
结 论
年轻人类/小鼠的CSF可以逆转降低的认知功能,这种能力可能是通过OPCs中的Fgf17实现的。这项研究为逆转衰老带来了新的曙光。
参考文献
Tal I, et al. Young CSF restores oligodendrogenesis and memory in aged mice via Fgf17. Nature, 2022. DOI: 10.1038/s41586-022-04722-0.
编译作者:KK(brainnews创作团队)
校审:Simon(brainnews编辑部)
- END -
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#少突胶质细胞#
41
#Nat#
37
#胶质细胞#
48
#细胞增殖#
55