Eur Radiol: 心房颤动患者左心耳血栓的诊断——延迟对比增强心脏CT
2021-03-15 shaosai MedSci原创
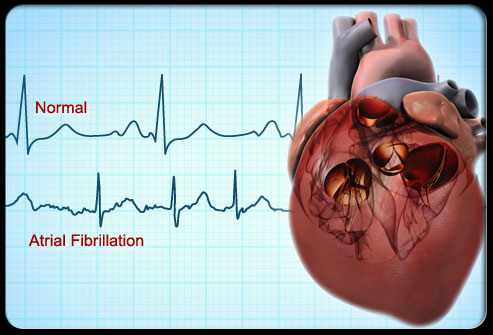
心脏计算机断层扫描(CCT)是一种成熟的评估左心房和肺静脉解剖的影像学技术。CCT影像可结合电生理图引导房颤(AF)导管射频消融。

心脏计算机断层扫描(CCT)是一种成熟的评估左心房和肺静脉解剖的影像学技术。CCT影像可结合电生理图引导房颤(AF)导管射频消融。此外,CCT作为一种新兴的检测左心耳(LAA)血栓的无创成像方式,已被作为射频导管消融前的常规检查,以降低随后血栓栓塞事件的发生风险。
虽然CCT是一种敏感性极高的排除心内血栓的影像学方法,但早期成像不能直观地区分循环淤积与LAA或其他心脏部位的血栓,因此特异性和阳性预测价值较低。已有研究表明,当延迟采集时间获取图像时,可以提高CCT诊断LAA血栓的准确性。然而,不同报告的诊断准确性差异很大,很难得出一个明确的结论,这限制了CCT在这种情况下的常规使用。此外,报道的延迟采集时间有很大差异,从30秒到3分钟不等,导致研究结果的特异性和阳性预测值(PPVs)之间存在明显差异。在这种情况下,经食管超声心动图(TEE)被国际指南推荐为诊断LAA血栓的唯一影像学方法,特别是对于持续性房颤患者,但其作为一种半侵入性检查很难在临床上广泛应用。
近日,发表在European Radiology杂志的一项研究以TEE为参考标准,开发了一种用于诊断房颤(AF)患者LAA血栓的心脏计算机断层扫描(CCT)的最佳方案。

前瞻性纳入260名因房颤接受射频消融治疗的连续患者。所有患者均在2小时内接受CCT和TEE检查。CCT方案包括一个标准的血管造影扫描和三个延迟扫描,延迟扫描分别在注射造影剂后1分钟、3分钟和6分钟。血栓被定义为延迟6分钟扫描时持续存在的充盈缺损。
TEE显示自发性强化52例(20%)、血栓10例(4%)。在63例(24%)患者中,CCT显示在血管造影扫描LAA的早期充盈缺损。其中,15人(6%)在1分钟时出现持续的充盈缺损,12人(5%)在3分钟时出现,10人(4%)在6分钟时出现。所有在TEE上诊断的10个血栓都通过延迟CCT正确识别,没有任何假阳性。对所有阶段,敏感性和阴性预测为100%。特异性从血管造影时的79%增加到6分钟时的100%。阳性预测值由16%提高到100%。血管造影扫描的估计辐射暴露为2.08±0.76 mSv(均值±标准差),每个延迟扫描的估计辐射暴露为0.45±0.23 mSv。

表1 延迟对比CCT和经食管超声心动图检测左心耳血栓的一致性。
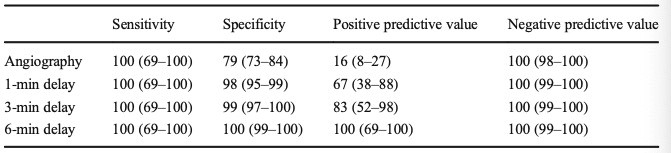
表2 对比剂注射后在不同时间获得的扫描诊断准确性参数。
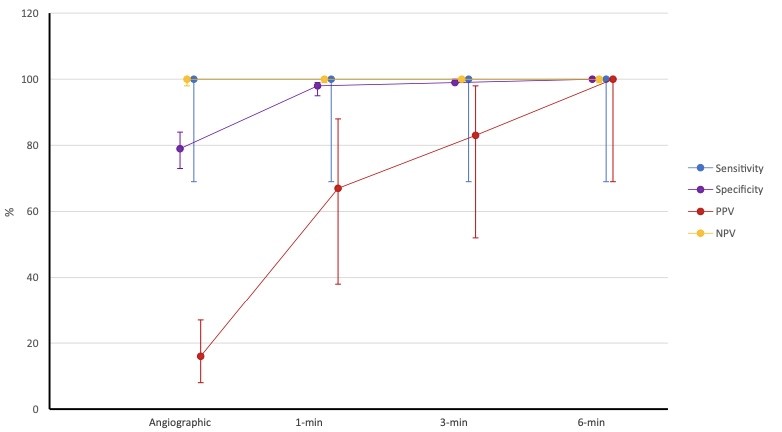
图1 不同CCT期相的诊断性能,表示为敏感性、特异性、阳性预测值(PPV)和阴性预测值(NPV)。
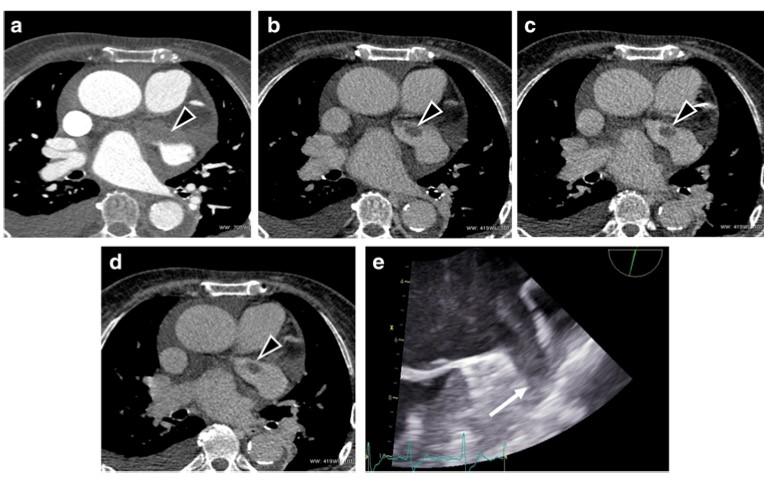
图2 一名53岁男子的轴位心脏图像。(a)早期阶段的CCT图像显示了LAA的充盈缺损(黑色箭头),并且在多次进行的后期扫描(b–d)中均存在少量持续性的充盈缺损,提示LAA内有血栓。(e)在CCT确认LAA血栓形成1小时后获得的TEE图像(白色箭头)。
本研究表明,在CCT扫描方案血管造影扫描后增加6分钟的延迟扫描是诊断LAA血栓的最佳方法,且辐射剂量较低。鉴于LAA血栓的患病率非常低,绝大多数患者的检测结果为阴性,因此CCT延迟扫描方案可作为常规TEE检查的替代性无创检查。
原始出处:
Pietro Spagnolo,Manuela Giglio,Daniela Di Marco,et al. Diagnosis of left atrial appendage thrombus in patients with atrial fibrillation: delayed contrast-enhanced cardiac CT.DOI:10.1007/s00330-020-07172-2
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言









#心脏CT#
42
好方法
70
#左心耳#
44
#心房#
54
每个人都接受CCT和TEE?患者接受度低
87
房颤,临床上碰到很多哦
60