Radiology:这一技术,让结直肠癌肺转移患者看到希望!
2021-05-05 shaosai MedSci原创
结直肠癌(CRC)是世界范围内最常见的恶性肿瘤之一,约有10%至20%的患者出现肺部转移。
结直肠癌(CRC)是世界范围内最常见的恶性肿瘤之一,约有10%至20%的患者出现肺部转移。当原发肿瘤和肺转移都可以完全切除时选择手术治疗,肺转移切除术后3年总生存率(OS)为53%–82%。对于不适合手术的患者进行全身化疗,但其三年OS率低于50%。立体定向放射疗法是CRC肺转移的另一种治疗选择,据报道3年OS率为43%–51%。
射频消融术(RFA)是另一种针对恶性肺肿瘤的微创局部治疗手段,是立体定向放射治疗的合理替代方案。对于不适合手术的CRC肺转移患者,RFA的OS率与立体定向放射治疗相当。
近日,发表在Radiology杂志的一项研究前瞻性评估了可切除结CRC肺转移患者行RFA的预后,为优化CRC肺转移患者的治疗流程提供了有价值的参考依据。
本项前瞻性多中心研究纳入的参与者需满足以下标准:肺转移病灶5个或以下、直径小于3厘米且手术可切除。从2008年1月到2014年4月本研究纳入的CRC患者共100个肺转移瘤,测量范围为0.4-2.8 cm(平均1.0 cm±0.5),共进行了88次RFA治疗。主要终点是3年总生存率(OS),预期为55%。以局部肿瘤进展率和安全性作为次要终点。OS率采用Kaplan-Meier法计算。通过单变量和多变量分析,采用Log-rank检验和Cox比例回归模型来确定预后因素。不良事件的评估依据不良事件通用术语标准3.0版。
本研究共纳入70例CRC患者(平均年龄66岁±10岁;49名男性)。3年OS率为84%(59/70例;95%置信区间[CI]: 76%, 93%)。在多变量分析中,与更低的OS相关的因素包括肿瘤位于直肠而非结肠(风险比[HR] = 7.7;95% CI: 2.6、22.6;P < .001)、癌胚抗原阳性(HR = 5.8;95% CI: 2.0, 16.9;P = .001)、无化疗史(HR = 9.8;95%CI: 2.5、38.0;P < .001)。70名参与者中有6名(9%)出现了局部肿瘤进展。88次RFA治疗中有一次出现了5级不良事件(1%),18次出现了2级不良事件(20%)。
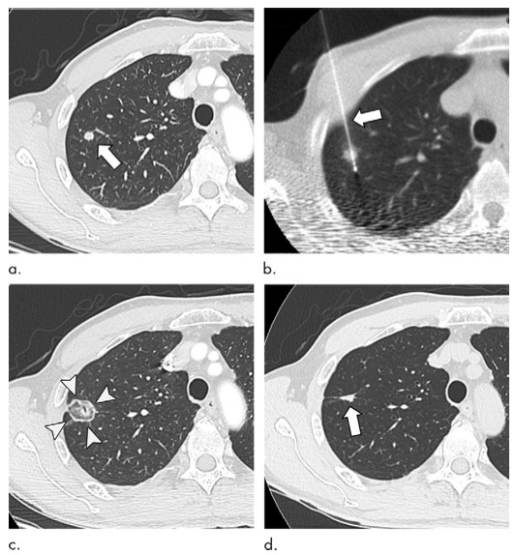
图1 64岁男性,结肠癌肺转移。(a)基线图像显示右肺上叶一个直径5mm肺的结节(箭头)。3个月后CT随访,结节增大至8mm,诊断为肺转移。(b)射频消融(RFA)采用冷却电极(箭头)。(c) RFA术后1个月CT图像显示肿瘤被消融区覆盖良好(箭头)。(d)射频消融7年后的图像。治疗后肿瘤变小,呈索条状(箭头)。
综上所述,本研究表明射频消融术可为患有可手术切除的3cm或更小的结直肠癌肺转移患者提供84%的3年良好预后效果,为临床进一步提高患者预后提供了参考依据。
原文出处:
Takaaki Hasegawa,Haruyuki Takaki,Hiroshi Kodama,et al.Three-year Survival Rate after Radiofrequency Ablation for Surgically Resectable Colorectal Lung Metastases: A Prospective Multicenter Study.DOI:10.1148/radiol.2020191272
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












学习
64
#结直肠#
38
#肺转移#
45
已阅
68