BMJ:肝素治疗可降低D二聚体水平升高的中度新冠肺炎住院患者死亡风险
2021-10-20 MedSci原创 MedSci原创
在中度Covid-19住院且伴有D-二聚体水平升高的患者中,接受治疗性肝素治疗可降低患者28天死亡风险,且出血风险较低

Covid-19住院患者临床病情恶化的最常见原因是低氧血症性呼吸衰竭,患者肺内皮损伤,形成微血管血栓,进而引发凝血功能障碍,最常见的临床指标为D-二聚体水平升高。肝素是临床上常用的抗凝血药物,还具有抗炎和潜在的抗病毒作用,可改善内皮功能。随机试验表明,治疗性肝素抗凝可能对中度Covid-19患者有益,但对危重症患者无效,提示开始肝素治疗的时间十分关键。近日研究人员考察了在中度Covid-19住院患中,治疗性肝素与预防性肝素治疗对患者预后的影响。
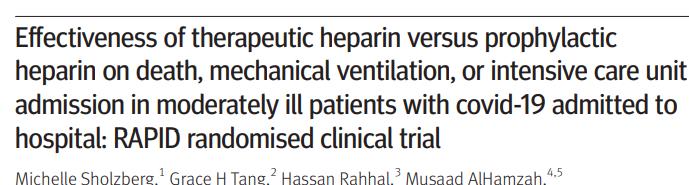
本次研究在巴西、加拿大、爱尔兰、沙特阿拉伯、阿拉伯联合酋长国和美国的28家医院开展,465名Covid-19且D-二聚体水平升高的住院成年患者参与,随机接受治疗剂量肝素(n=228)或预防剂量肝素(n=237)治疗,持续到出院、第28天或死亡。研究的主要终点为死亡、有创机械通气、无创机械通气或入住重症监护病房,次要终点包括全因死亡、全因死亡或任何机械通气的复合终点,静脉血栓栓塞。安全性结果包括大出血。
参与者的平均年龄为60岁,264名(56.8%)为男性,平均体重指数为30.3 kg/m2。28天时,228名接受治疗性肝素治疗的患者中37人出现主要终点(16.2%),而237名接受预防性肝素治疗的患者中52出现主要终点事件(21.9%),风险比为0.69。4名接受治疗性肝素治疗的患者死亡(1.8%),接受预防性肝素治疗的患者中18名死亡,死亡风险比0.22。23名(10.1%)接受治疗性肝素治疗的患者和38名(16.0%)接受预防性肝素治疗的患者(0.59)出现了全因死亡或任何机械通气的复合终点。2名接受治疗性肝素治疗的患者(0.9%)发生静脉血栓栓塞,预防性肝素治疗组6名(2.5%),风险比0.34。2名(0.9%)接受治疗性肝素治疗的患者和4名(1.7%)接受预防性肝素治疗的患者发生大出血(风险比0.52)。
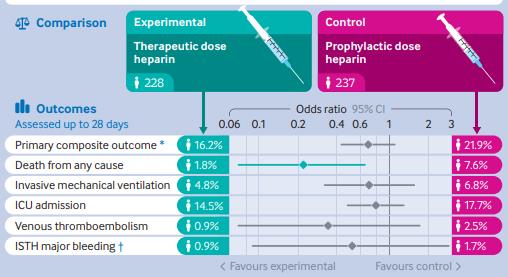
肝素治疗对患者预后的影响
研究发现,在中度Covid-19住院且伴有D-二聚体水平升高的患者中,接受治疗性肝素治疗可降低患者28天死亡风险,且出血风险较低。
原始出处:
Michelle Sholzberg et al. Effectiveness of therapeutic heparin versus prophylactic heparin on death, mechanical ventilation, or intensive care unit admission in moderately ill patients with covid-19 admitted to hospital: RAPID randomised clinical trial BMJ. 14 October,2021.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#肝素治疗#
39
#患者死亡#
48
#二聚体#
45
#BMJ#
31
#死亡风险#
42