曹雪涛院士:1篇PNAS,1篇Cancer Cell
2016-08-17 佚名 生物探索
导语:曹雪涛院士是我国著名的免疫学家。7月25日,小编曾在《曹雪涛院士:5个月发表7篇“免疫与癌症”相关论文及综述》一文中汇总了今年3月-7月曹院士发表的部分研究成果。转眼间8月已过半,小编注意到,曹雪涛院士带领的团队相继在Cancer Cell、PNAS上发表了2项新的研究成果。Cancer Cell揭秘癌症转移机制Tumor Exosomal RNAs Promote Lung Pre-met
导语:曹雪涛院士是我国著名的免疫学家。7月25日,小编曾在《曹雪涛院士:5个月发表7篇“免疫与癌症”相关论文及综述》一文中汇总了今年3月-7月曹院士发表的部分研究成果。转眼间8月已过半,小编注意到,曹雪涛院士带领的团队相继在Cancer Cell、PNAS上发表了2项新的研究成果。

Cancer Cell揭秘癌症转移机制
Tumor Exosomal RNAs Promote Lung Pre-metastatic Niche Formation by Activating Alveolar Epithelial TLR3 to Recruit Neutrophils
8月8日,发表在Cancer Cell上的一项研究中,来自第二军医大学、中国医学科学院的科学家小组证实,肿瘤外泌体RNAs能够通过激活肺泡上皮细胞中的Toll样受体3(Toll-like receptor 3, TLR3)招募中性粒细胞,从而促进肺部转移前微环境(pre-metastatic niche)的形成。曹雪涛院士是这一研究的通讯作者。
肿瘤转移是癌症相关死亡的主要原因。在这一过程中,癌细胞会扩散到其它器官,并适应新的环境。肿瘤与其微环境之间的协作驱动了这些过程。原发性肿瘤能够通过促进转移前微环境的形成转变为继发性肿瘤。
这一过程涉及了多种肿瘤分泌因子、宿主基质微环境以及骨髓来源细胞之间的交互作用。原发性肿瘤与不同器官之间交互作用背后的机制是一个需要被充分理解的重要问题。
近年来,研究发现,TLRs能够促进多种肿瘤进程,包括肿瘤发生、生长和转移。宿主TLRs能够启动慢性炎症反应促进肿瘤发生,而肿瘤细胞TLRs能够提供抗凋亡和增殖信号,支持肿瘤的生长和侵袭。
尽管TLRs调节肿瘤转移背后的机制吸引了很多科学家注意。但由于相关研究使用了不同的转移模型和细胞,宿主TLRs在癌症转移中的作用是有争议的。
在这一研究中,科学家们想要确定,一旦被肿瘤来源因子(tumor-derived factors)激活,宿主间质细胞TLRs会如何帮助启动转移前炎症反应和转移前微环境的形成。
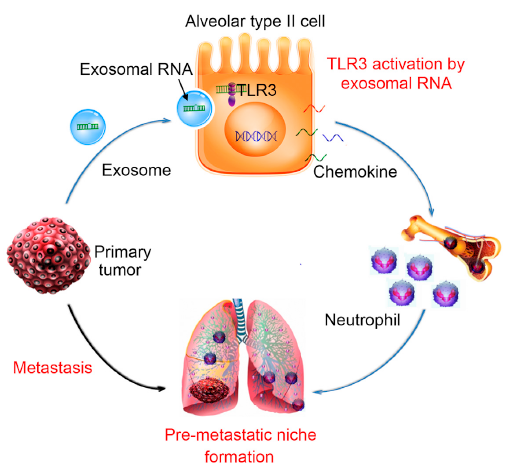
研究证实,肺上皮细胞能够通过TLR3感知肿瘤外泌体RNAs,这对启动中性粒细胞招募和肺转移微环境的形成至关重要。研究发现,在自发性转移模型中,TLR3缺陷小鼠肺转移会减少。
研究人员进一步揭示了这一现象背后的机制,结果证明,原发性肿瘤来源的外泌体RNAs在肺上皮细胞中激活了TLR3,从而诱导了肺部趋化因子的分泌,促进了中性粒细胞的招募。这一研究成果为控制癌症向肺部转移提供了潜在的靶点。
PNAS发表重要免疫学成果
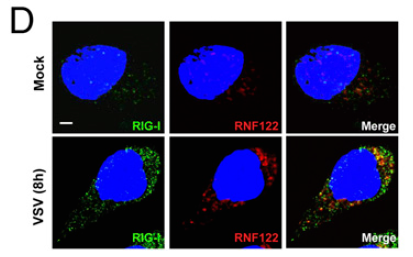
RNF122 suppresses antiviral type I interferon production by targeting RIG-I CARDs to mediate RIG-I degradation
8月9日,来自中国医学科学院、军事医学科学院的科学家小组在《美国国家科学院院刊》(PNAS)上发表了一项免疫学重要成果。曹雪涛院士及军事医学科学院基础医学研究所的张纪岩(Jiyan Zhang)是这篇论文的共同通讯作者。
先天免疫是宿主抵御感染的第一道防线。先天免疫的激活与病原体相关的分子模式(pathogen-associated molecular patterns,PAMPs)的检测有关,如微生物的核酸、蛋白质、脂脂质和碳水化合物。PAMPs是通过模式识别受体(pattern recognition receptors,PRRs)被识别出来的,包括Toll样受体、RIG-I样受体(retinoic acid-inducible gene 1 (RIG-I)–like receptors)、NOD样受体以及C型凝集素受体。
RIG-I是细胞质病毒RNA传感器,能够触发信号,诱导I型干扰素和促炎细胞因子的产生,响应病毒感染。RIG-I信号的精准控制对有效清除病毒,并不产生有害的免疫病理反应至关重要。如何及时地终止RIG-I信号,预防I型干扰素的过量产生,避免引发炎症免疫性疾病等问题需要被研究清楚。
翻译后修饰(尤其是泛素化)在RIG-I活性调节中扮演着关键的角色。研究发现,E3泛素连接酶参与了RIG-I信号的调节。RNF家族是E3泛素连接酶的主要家族之一。近期,科学家们发现,多个RNF蛋白与先天免疫调节相关。在这一研究中,为了鉴定出直接与RIG-I产生作用,以及负调节RIG-I活性的蛋白,研究小组结合了免疫沉淀反应和多维MS分析。结果发现,E3泛素连接酶RNF122能够直接绑定小鼠RIG-I的激活和招募域(activation and recruitment domains, CARDs),调节RIG-I K48连接的泛素化,最终,通过促进RIG-I蛋白酶体降解抑制RIG-I依赖的抗病毒反应。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#CEL#
50
#PNAS#
42
#cancer cell#
44
学习一下,好
93
这篇资讯带给我们新知识,启发新思维,不论是科研还是临床工作都有很大的帮助。。。
78
顶一个,曹爷爷
88
值得学习
85
值得学习
75
#曹雪涛#
33
#Cell#
29