Nat Commun:SOX2/GLI1-ST3GAL1-AXL通路促进黑色素瘤的转移
2020-11-28 xiaozeng MedSci原创
恶性黑色素瘤是皮肤癌中最具侵袭性和治疗抗性的形式。其侵袭性主要是因为即使在疾病的早期,黑色素瘤细胞仍具有高度转移性。
恶性黑色素瘤是皮肤癌中最具侵袭性和治疗抗性的形式。其侵袭性主要是因为即使在疾病的早期,黑色素瘤细胞仍具有高度转移性。
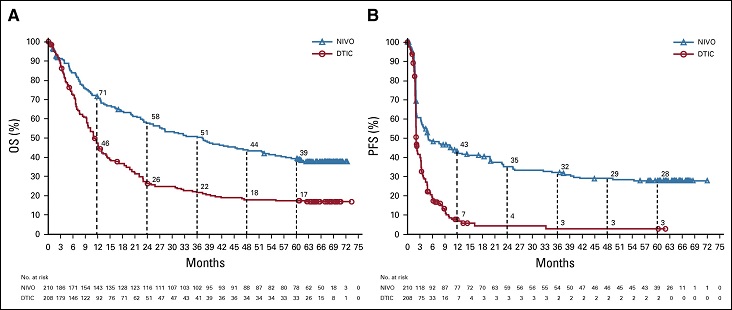
尽管最新的治疗进展显示,在一小部分晚期黑素瘤患者中,靶向疗法和免疫检查点抑制剂能够实现患者的长期生存,但转移性黑色素瘤仍是一种无法治愈的疾病。因此,识别和靶向黑色素瘤转移的关键驱动因素对于有效控制肿瘤发生发展至关重要。
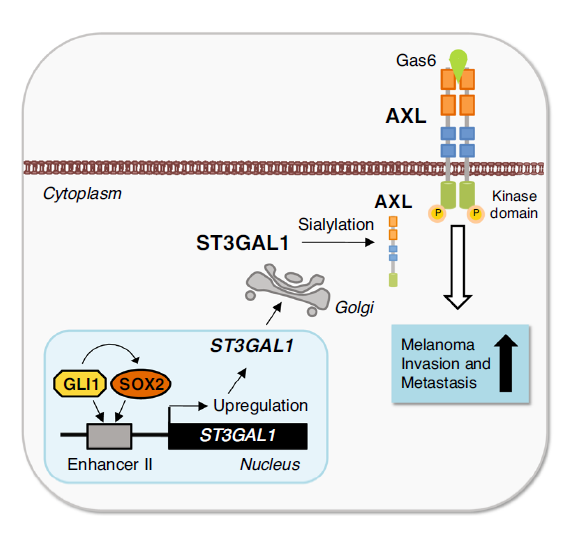
SOX2/GLI1-ST3GAL1-AXL通路的作用机制
在该研究中,研究人员报告了一种机制,即致癌的SOX2-GLI1转录复合物能够通过介导唾液酸转移酶ST3GAL1进而调控黑色素瘤的侵袭作用。进一步的研究显示,ST3GAL1能够驱动黑色素瘤的转移。沉默该酶可以抑制黑色素瘤的侵袭作用,并显著降低侵袭性黑色素瘤细胞进入血流,定植于远端器官,并在转移环境中生存的能力。
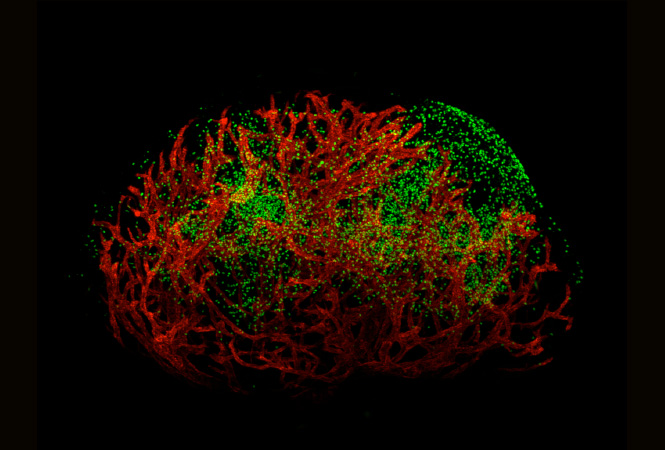
ST3GAL1在皮肤黑色素瘤中的表达及其与黑色素瘤发生发展的关系
糖基化蛋白分析结果显示,受体酪氨酸激酶AXL是ST3GAL1侵袭性功能的主要效应因子。ST3GAL1能够诱导AXL的二聚化和激活,进而促进黑色素瘤的浸润作用。
总而言之,该研究结果显示,ST3GAL1-AXL通路是驱动黑色素瘤转移的关键,靶向该通路或可成为转移性黑色素瘤的潜在治疗策略。
原始出处:
Pietrobono, S., Anichini, G., Sala, C. et al. ST3GAL1 is a target of the SOX2-GLI1 transcriptional complex and promotes melanoma metastasis through AXL. Nat Commun 11, 5865 (17 November 2020).
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#Sox2#
29
#COMMUN#
35
#色素#
29
#Nat#
29
新的方向呀
72
#黑色素#
32
#黑色素#
23
ST3GAL1-AXL通路促进黑色素瘤的转移
77