Clin Cancer Res:纳武单抗+伊匹单抗+英夫利昔单抗/赛妥珠单抗治疗黑色素瘤
2021-01-06 Nebula MedSci原创
对于晚期黑色素瘤患者,TNF阻滞剂可用于处理纳武单抗和/或伊匹单抗治疗后的胃肠道炎症副作用。临床前数据显示,抗-TNF可以提高免疫检查点抑制剂的疗效。
对于晚期黑色素瘤患者,TNF阻滞剂可用于处理纳武单抗和/或伊匹单抗治疗后的胃肠道炎症副作用。临床前数据显示,抗-TNF可以提高免疫检查点抑制剂的疗效。
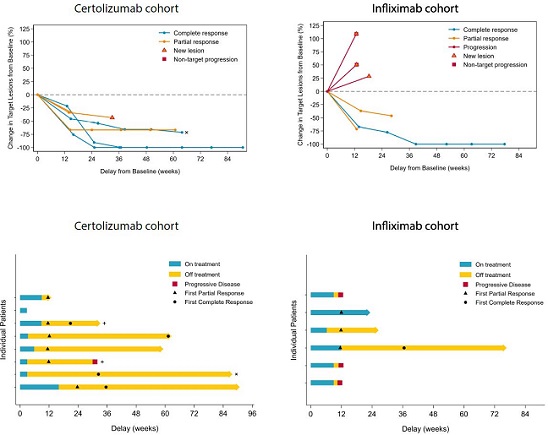
TICIMEL (NTC03293784)研究是一项开放标签、双臂的Ib期临床试验,招募了14位晚期和/或转移性黑色素瘤患者(IIIc/IV期),接受纳武单抗(1 mg/kg)和伊匹单抗(3 mg/kg)联合英夫利昔单抗(5 mg/kg,n=6)或赛妥珠单抗(400/200 mg,n=8)。主要终点是安全性,次要终点是抗肿瘤活性。
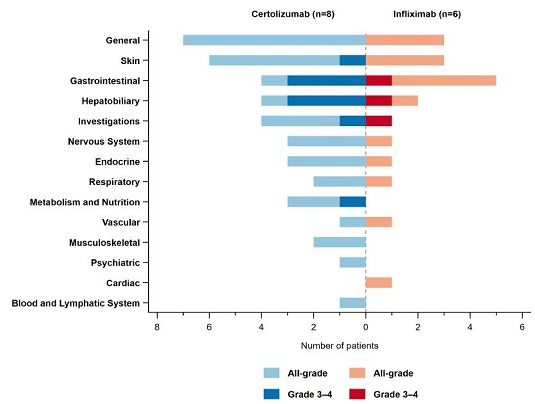
在英夫利昔单抗队列中仅观察到一例剂量限制性毒性(DLT)。这两种不同的联合方案的安全性都良好。与赛妥珠单抗相比,英夫利昔单抗治疗相关的不良反应较少。
在赛妥珠单抗队列中,有一位患者未纳入治疗应答分析。在该队列中,8位患者中有4位表现出肝胆功能障碍,7位可评估患者全部获得了客观缓解(OR),包括4例完全缓解(CR)和3例部分缓解(PR)。在英夫利昔单抗队列中,有1例CR和2例PR,另外3位患者病程进展(PD)。在两组患者中均观察到了系统性T细胞反应的激活和成熟的迹象。
总之,该研究表明,这两种联合方案用于晚期黑色素瘤患者的安全性良好,而且表现出一定的临床和生物学活性。赛妥珠单抗队列的患者的高缓解率值得进一步研究。
原始出处:
Anne Montfort, et al. Combining Nivolumab and Ipilimumab with Infliximab or Certolizumab in Patients with Advanced Melanoma: First Results of a Phase Ib Clinical Trial. Clin Cancer Res January 5 2021 DOI:10.1158/1078-0432.CCR-20-3449
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#色素#
42
#赛妥珠单抗#
44
#黑色素#
39
#黑色素#
42