European Heart Journal:少量饮酒也会增高房颤发生风险!不论啤酒、白酒与红酒
2021-01-20 “心关注”公众号 “心关注”公众号
作为严重影响公众健康的心律失常疾病类型之一,房颤在人口老龄化社会中的发病率不断增高,并与患者的不良预后密切相关,包括卒中、房颤等,也使得患者的死亡风险增高两倍以上。
作为严重影响公众健康的心律失常疾病类型之一,房颤在人口老龄化社会中的发病率不断增高,并与患者的不良预后密切相关,包括卒中、房颤等,也使得患者的死亡风险增高两倍以上。
一 饮酒增加心率失常发生率
从病理生理角度看,酒精可能对心律失常的发生存在直接影响,假日心脏综合征(节假日过量饮酒后,出现以心律失常为主的一系列临床症状)就是很典型的案例。
德国慕尼黑大学 Stefan Brunner 教授团队曾探究饮酒与心律失常的相关性,并于 2017 年将结果发表在了《European Heart Journal》杂志上。研究纳入了慕尼黑啤酒节的 3028 名志愿者作为急性饮酒组,奥格斯堡 KORA S4 研究中的 4131 名社区志愿者作为慢性饮酒组,使用智能手机心电图检测参与者的心律失常情况。
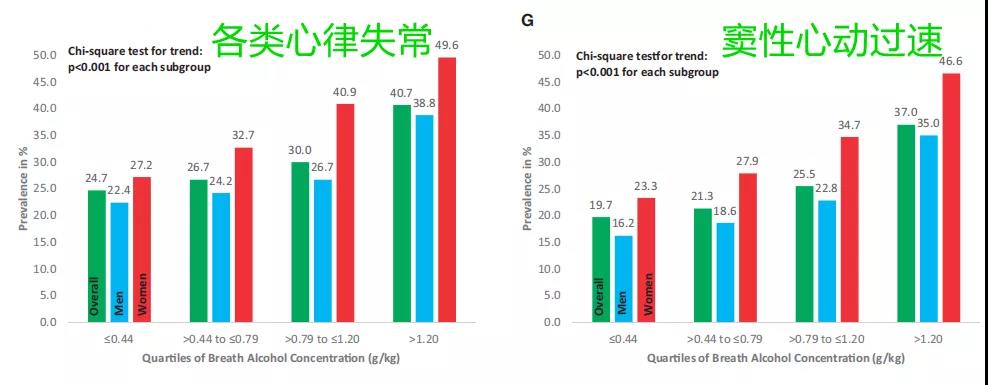
在急性饮酒组中,依据呼气酒精浓度(BAC)对受试者进行分组,可观察到,随着 BAC 的升高,受试者心律失常(总)和窦性心动过速的发生率均显着升高。
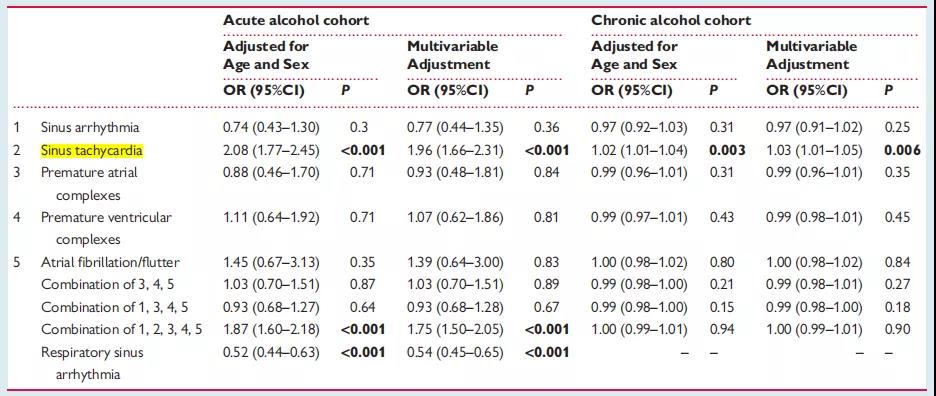
在经过包括年龄、性别在内的多变量校正后,发现窦性心动过速与急性饮酒、慢性饮酒均存在显着关联,分析结果见下述表格:
二 饮酒与房颤发生风险
已有诸多研究验证了男性中重度饮酒与房颤发生发展的关系。谈及女性,四大医学杂志之一的《JAMA》杂志,既往曾发表过女性饮酒与房颤发生风险的相关研究。
该研究纳入了美国妇女健康研究(WHS)中的 34,715 位初始状况健康的女性,分 4 组(不饮酒、每天饮酒 1 杯以内、每天 1-2 杯、每天 2 杯以上),经中位时间 12.4 年的随访,共确诊 653 例房颤。
根据患者不同的基线特征进行分层后发现:每天饮酒 2 杯以内的女性,房颤发生风险与不饮酒的女性无显着差异;每天饮酒 2 杯以上的女性,房颤发生风险是不饮酒女性的 1.67 倍。
在年龄>60 岁、不吸烟、非高血压或非高脂血症的女性人群中,每天饮酒 2 杯以上与不饮酒女性相比,房颤发生风险的差异表现得更为明显。相关数据如下:

三 Meta分析:轻中重度饮酒与房颤
虽然已经明确了重度饮酒患者的房颤发病风险更高,轻中度饮酒对房颤发病率的影响,尚有待进一步合并分析。
2017 年澳大利亚皇家阿德莱德医院Prashanthan Sanders教授团队发表在《International Journal of Cardiology》的meta分析,探究了轻中重度饮酒与房颤发病风险的关联。
在轻度饮酒组中,与不饮酒组相比,无论男(HR=1.01,95%CI 0.82-1.24,P=0.93)、女(HR=0.93,95%CI 0.82-1.05,P=0.25)的房颤发病风险,均未表现出显着差异。
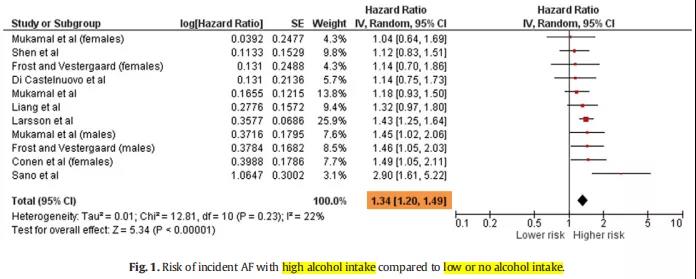
在合并 11 项临床研究后,发现重度饮酒组的房颤发生率,显着高于不饮酒/轻度饮酒组(HR=1.34,95%CI 1.20-1.49,P<0.00001),森林图如下:
在中度饮酒组中,仅男性的房颤发生风险显着增高(HR=1.26,95%CI 1.04-1.54,P=0.02),未观察到女性的显着差异,森林图分析结果如下:

此外,重度饮酒组男女性的房颤发病风险均显着增高,这与既往多数研究的结论相一致。
四 适度饮酒降低心衰风险
饮酒与房颤发病风险之间的机制效应,尚不是十分明确。值得一提的是,对于与房颤发生发展关系密切的疾病,比如心衰、冠心病等,轻中度饮酒似乎可以降低此类疾病的发病风险。
2017 年发表在《JACC-Heart Failure》上的意大利研究发现,适度饮酒可降低心衰发病风险。
具体到各亚组分层,在地中海饮食依从性高(评分> 4 分)、高收入(>25000 欧元/年)或中高等教育群体里,部分饮酒量组别已经表现出了显着性差异:

五 欧洲心脏杂志最新研究
基于在轻度饮酒人群中,酒精摄入量与房颤发生率关联的争议性。德国汉堡大学心脏和血管中心 Renate B Schnabel 教授团队进一步研究了轻度饮酒与房颤的关系,并于 2021 年 1 月 13 日将结果发表在了《European Heart Journal》杂志上。
该队列研究纳入了欧洲多国的 107,845 例受试者,年龄中位数 47.8 岁,男性占比 48.3%,酒精摄入量中位数是 3 g/天。
经过中位时间 13.9 年的随访,共有 5854 例受试者确诊房颤。通过 Cox 回归分析发现,酒精摄入量与房颤发生风险呈非线性正向相关关系。与之相反的是,轻度饮酒与心衰风险的降低相关联。
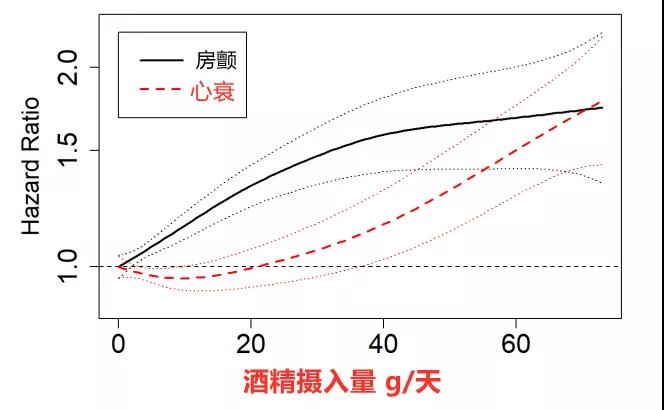
每天饮酒 1 杯(酒精摄入量12 g)时,风险比HR为 1.16(95%CI 1.11-1.22,P < 0.001),意味着房颤风险增加 16%;每天饮酒 2 杯时,房颤风险增加 36%;每天饮酒 3 杯时,房颤风险增加 52%。
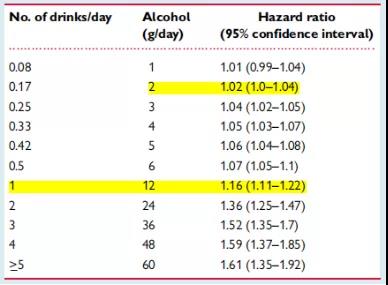
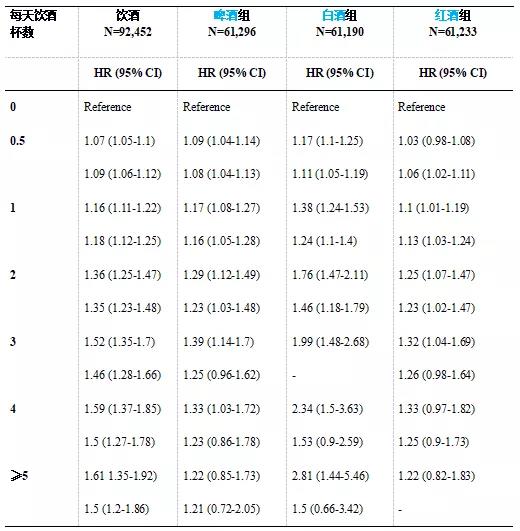
不同酒类,包括啤酒、白酒和红酒,均可显着增加房颤发生风险。这种相关性,各酒类之间的差异不大,以白酒(烈酒)最为明显。
另外,研究还排除了生物标注物 hsTnI、Nt-proBNP 的浓度水平对饮酒致房颤风险增高的影响。
六 研究结论
饮酒与房颤的发生风险呈正相关关系,这种关联与经典的病理生理路径无关。
尽管少量饮酒可降低其他心血管疾病(比如心衰)的发生风险,最新研究发现,从非常低的日酒精摄入量开始,涵盖各种酒类,饮酒就与房颤发生风险的增加相关联。
未来,有必要将患者的饮酒情况这一指标,添加到房颤的患病风险评估和预防策略中。
原始出处:
Dora C, Ngoc-Anh S, et al. Alcohol consumption, cardiac biomarkers, and risk of atrial fibrillation and adverse outcomes. European Heart Journal. 2021,13,January.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言











#PE#
24
酒是不能喝的
59
#ART#
22
#红酒#
40
#增高#
0
#HEART#
29
#增高#
26
已经痛风了
70
房颤,临床上碰到很多哦
36
未来,有必要将患者的饮酒情况这一指标,添加到房颤的患病风险评估和预防策略中。
58