J Cell Biochem:外泌体circ_0044516能够促进前列腺癌细胞增殖和转移
2019-10-30 Alex Yang MedSci原创
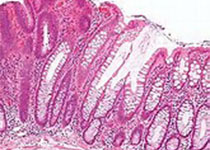
环状RNA(circRNAs)是癌症生长和恶化的重要调控因子。外泌体携带各种各样分子,包括RNA、蛋白和从一个细胞到另一个细胞的脂质。但是来自前列腺癌患者的外泌体circRNAs的作用仍旧不清楚。最近,有研究人员发现circ_0044516在前列腺癌中表达上调,并调查了Hsa_circ_0044516 (circ_0044516)的分子机制。首先,研究人员从前列腺癌患者中收集了外泌体,并进行人类c
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













很有用处!
77
#Bio#
31
#CEL#
42
#Cell#
35
#癌细胞增殖#
45
#癌细胞#
39
#细胞增殖#
38
#前列腺癌细胞#
36
学习了!
89
前列腺癌相关研究,学习了,谢谢梅斯
47