Neurology:脑血管反应性是脑淀粉样血管病核心特征,或为评估疾病严重程度、认知损害的生物标志物
2022-03-13 Naomi MedSci原创
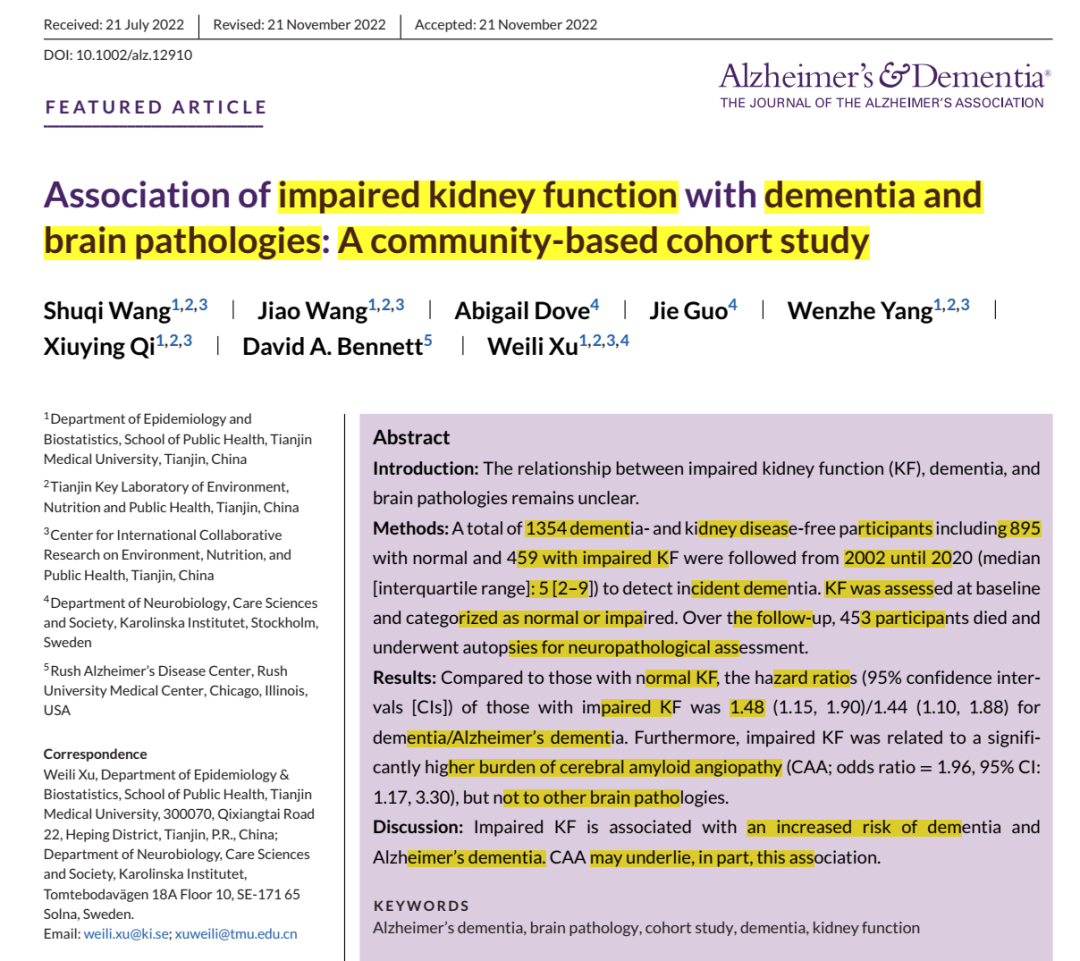
近日,有研究人员评估了CAA患者在高二氧化碳气体刺激下的全脑CVR,研究发现脑血管反应性降低是脑淀粉样血管病的核心特征,其评估可能为疾病严重程度和认知损害提供额外的生物标志物。
脑淀粉样血管病(CAA)是一种小血管病,由淀粉样β蛋白(Aβ)沉积在脑部小血管和软膜的中膜和外膜引起。它导致5-20%的脑出血(ICH),是公认的引起脑微出血(CMBS)、推测血管起源的白质病变、皮质浅铁质沉着(CSS)、血管周围间隙扩张和微梗死的原因。
在CAA患者中,出血(ICH、CMBS和CSS)和缺血性(白质病变和微梗死)后果的更大负担与认知障碍有关。另一个潜在的机制是脑血管反应性(CVR)降低,这限制了大脑区域在需要时接受更高血流量的能力。在CAA7转基因小鼠模型和CAA患者中都观察到CVR降低,但其与CAA神经影像标志物和CAA认知功能的关系尚不清楚。此外,CAA患者较低的CVR仅观察到对视觉任务的反应导致通过大脑后动脉的血流减少,在标准化屏气测试中通过大脑后动脉和大脑中动脉的血流增加,以及在视觉任务期间血氧水平依赖(BOLD)功能MRI的反应幅度较低。目前还没有关于CVR减少在整个大脑中的分布的数据,也没有关于灰质和白质CVR可能如何与CAA的出血、缺血和认知后果相关的数据。
阿尔茨海默病(AD)与CAA有许多共同的病理生理联系。两者均以Aβ积聚为特征,AD病理可能与CAA病理共存,范围从单纯血管性Aβ沉积到仅实质Aβ“纯”AD的沉积特征。一些研究表明,与健康对照组相比,阿尔茨海默病患者的CVR较低。因此,必须考虑并发AD病理可能加速CAA患者的CVR降低和认知损害。近日,有研究人员评估了CAA患者在高二氧化碳气体刺激下的全脑CVR,比较CAA患者、轻度认知障碍和AD患者和健康对照组之间的CVR,并探讨CVR与CAA的MRI标志物和认知功能的关系。
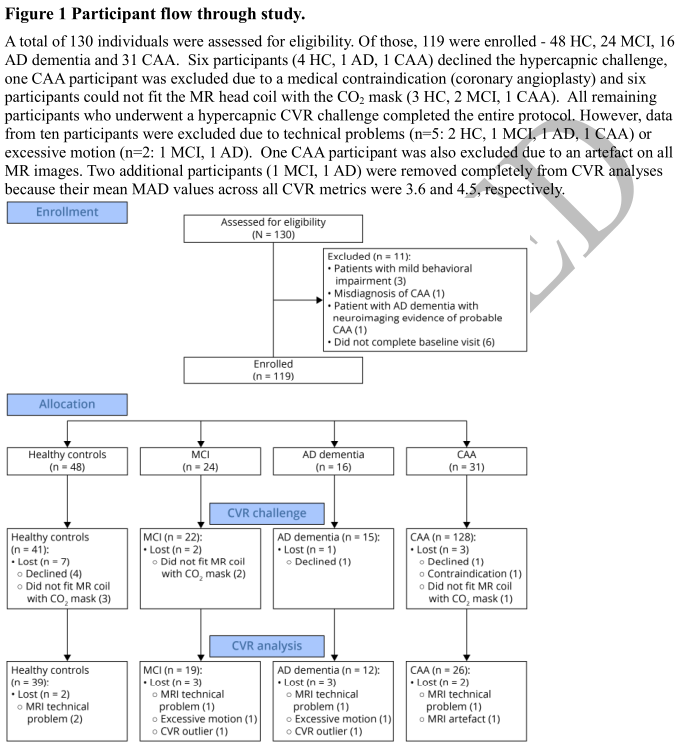
在这项横断面研究设计中,可能患有大脑淀粉样血管病、轻度认知障碍、阿尔茨海默病痴呆的患者和健康对照组接受了神经心理测试和核磁共振成像,其中包括5%的二氧化碳挑战。在控制了年龄、性别和高血压的组间比较了脑血管反应性,并通过调整了组、年龄、性别、教育程度和高血压的多变量线性回归,确定了脑血管反应性与脑淀粉样血管病患者的脑淀粉样血管病的MRI标志物以及所有参与者的认知之间的关系。
- 脑淀粉样血管病患者26例(女性9例,年龄74.4±7.7岁),轻度认知障碍患者19例(女性5例,年龄72.1±8.5岁),阿尔茨海默病痴呆患者12例(女性4例,年龄69.4±6.6岁),健康对照组39例(女性30例,年龄68.8±5.4岁)。
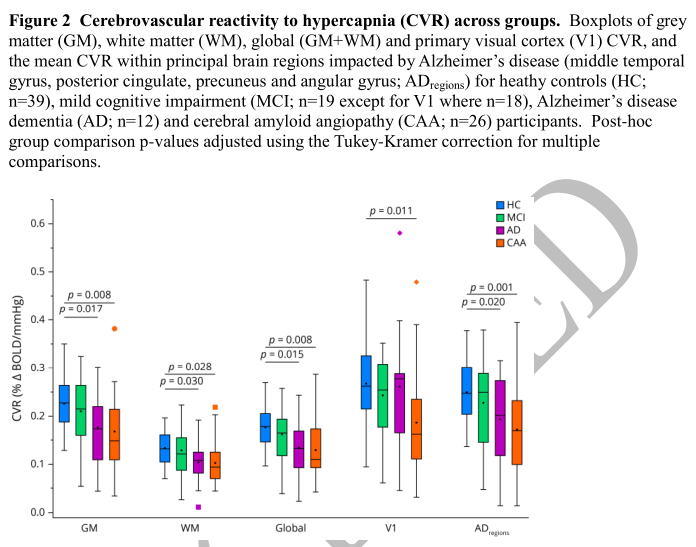
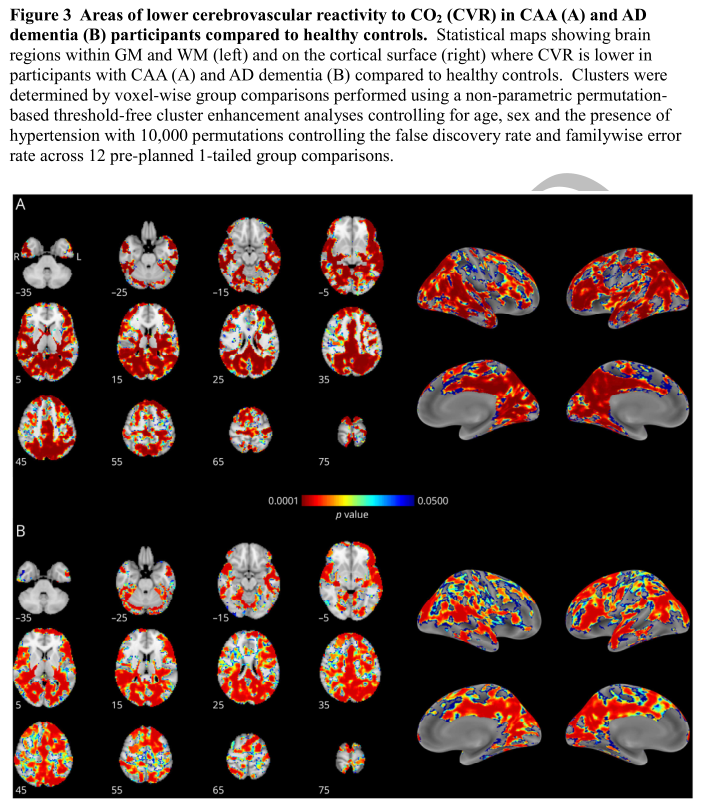
- 与健康对照组相比,患有脑淀粉样血管病和阿尔茨海默病痴呆症的参与者整个大脑的平均灰质和白质反应性较低,两组中反应性较低的主要分布在后方。
- 较高的白质高信号体积与较低的白质反应性相关(标准化系数[β],95%置信度区间):-0.48,-0.90到-0.01。
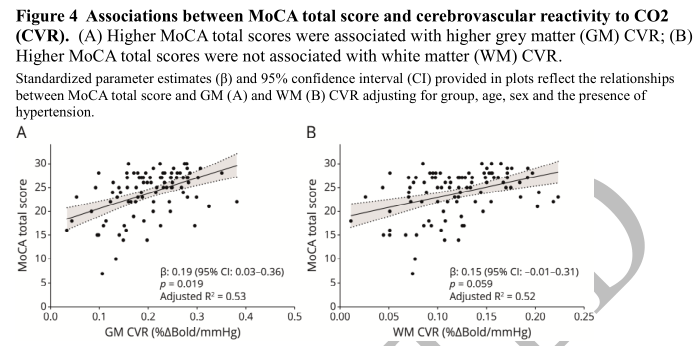
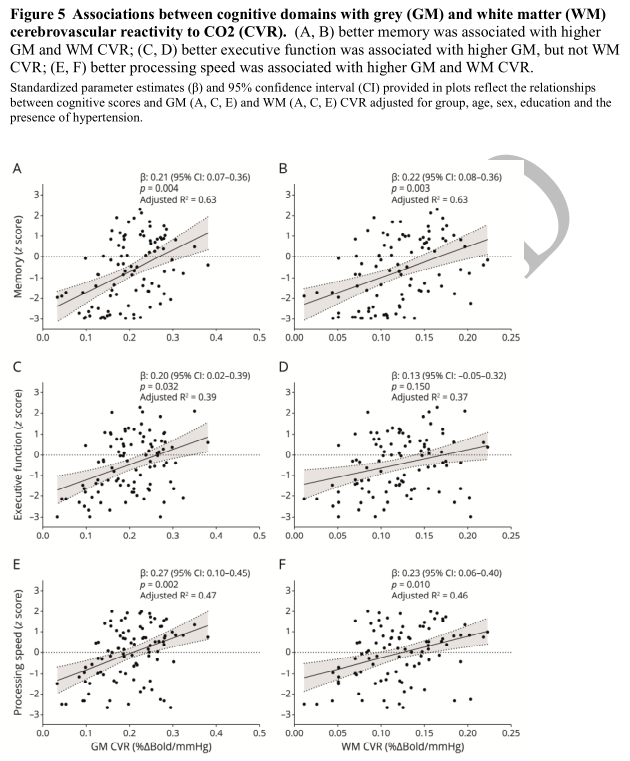
- 较高的灰质反应性与较好的整体认知功能(β:0.19,0.03~0.36)、记忆(β:0.21,0.07~0.36)、执行功能(β:0.2,0.02~0.39)和加工速度(β:0.27,0.10~0.45)相关;较高的白质反应性与较高的记忆力(β=0.22,0.08~0.36)和较高的加工速度(β=0.23,0.06~0.40)相关。
脑血管反应性降低是脑淀粉样血管病的核心特征,其评估可能为疾病严重程度和认知损害提供额外的生物标志物。
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言















#脑血管反应性#
54
#标志物#
42
#Neurol#
50
#脑淀粉样#
58
#血管病#
54
#反应性#
63
不错👍
55
#生物标志#
40
#生物标志#
39
#脑淀粉样血管病#
58