导语:十月怀胎,一朝分娩。
多年来,产后出血始终是严重的产后并发症及导致产妇死亡的主要原因。为降低产后出血的风险,各种指南均建议预防性地使用宫缩剂。过去的十年中,除宫缩剂外,氨甲环酸也被应用于预防产后失血的情况。氨甲环酸通过阻断纤溶酶原分子上的赖氨酸结合位点,有效地阻止了纤维蛋白溶解,从而达到促进止血的作用。除此之外,氨甲环酸在其他方面的临床作用也获得了证据支持,例如已发现它可以减少择期手术中的输血需求,并降低颅外或轻至中度颅内创伤患者的死亡率。
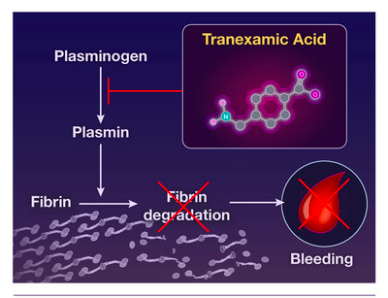
氨甲环酸还可以降低与产后出血相关的产妇死亡率。不仅如此,与这些妇女早期服用该药物有关的生存获益表明,比起治疗作用,氨甲环酸对分娩后凝血症的预防作用更优越。
研究人员在先前的试验中研究了预防性应用氨甲环酸在阴道分娩时的作用,发现在已经接受了预防性宫缩剂应用的产妇身上,氨甲环酸对产后出血的发生率并没有明显的作用。一项小型,单剂量中心,随机对照试验显示,对接受选择性剖宫产的妇女使用预防性氨甲环酸,可以大大减少失血量。 然而,由于与盲法,结果评估,耗损偏倚以及出院后随访(尤其是血栓栓塞事件)相关的方法学局限性,这些试验的结果被认为是不确定的,并且当前的指南不主张在剖宫产后常规给予氨甲环酸。由此,研究人员设计了以下试验,以确认剖宫产后预防性联合使用宫缩剂与氨甲环酸的产后出血的发生率是否比单独使用宫缩剂低。
在一项多中心,双盲,随机,对照试验中,研究人员将在分娩前或妊娠34周或更早的时候接受剖宫产的孕妇分配至两组,一组接受静脉注射预防性宫缩剂和氨甲环酸(1g),一组接受安慰剂治疗。 主要结局为产后出血,定义为产后2天之内计算出的估计失血量超过1000毫升或接受红细胞输血。 次要结果包括按重量估算的失血量,提供者评估的临床上明显的产后出血,使用其他子宫收缩剂和产后输血的情况。
实验结果表明,在接受随机分组的4551名女性中,有4431名接受了剖宫产,其中4153名(93.7%)拥有主要结的局数据。氨甲环酸组的2086名妇女中有556名(26.7%)发生了产后出血,安慰剂组的2067名妇女中有653名(31.6%)发生了产后出血(调整后的风险比为0.84; 95%的置信区间[CI]为0.75至0.94。P = 0.003)。而对于体重测定的平均失血量或提供者评估的临床上具有重大临床意义的产后出血,两组之间无显着差异。分娩后3个月内发生血栓栓塞事件,氨甲环酸组中0.4%(2049名中的8名)的产妇及安慰机组中0.1%(2056名中的2名)的产妇在分娩后三个月内发生了血栓栓塞事件(调整后的风险比为4.01; 95%的CI为0.85至 18.92;P=0.08)。
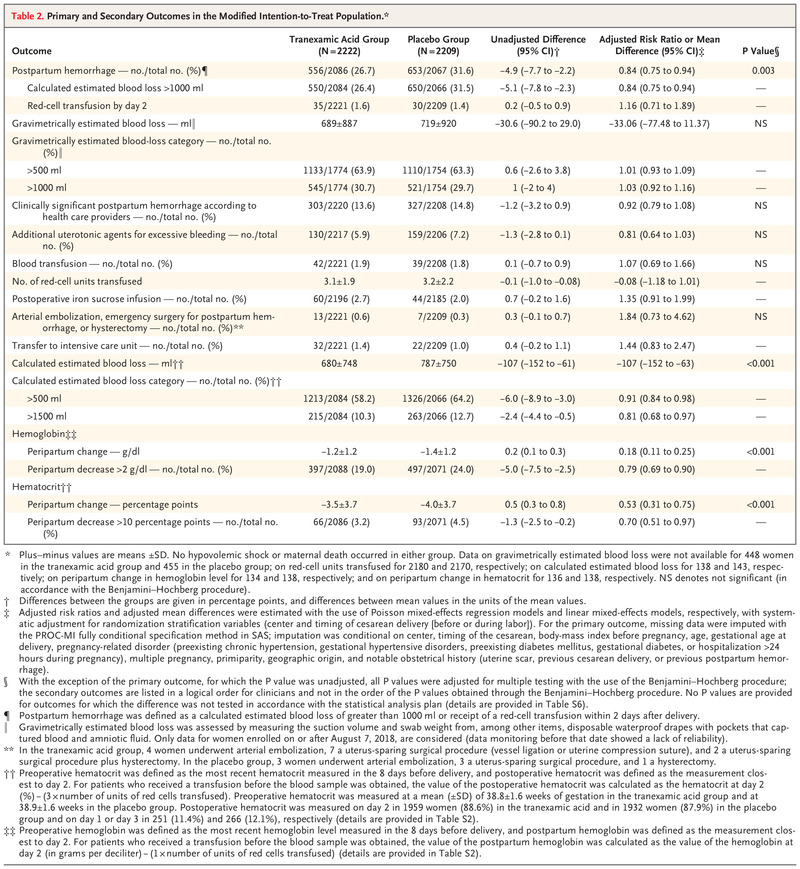
实验结果表明,在接受剖宫产并接受预防性宫缩剂治疗的产妇中,氨甲环酸治疗导致在第2天的估计失血量大于1000ml或需要红细胞输注的发生率显着低于安慰剂,但并未改善与出血有关的继发性临床结局。
原文链接:https://www.nejm.org/doi/full/10.1056/NEJMoa2028788?query=featured_home
Tranexamic Acid for the Prevention of Blood Loss after Cesarean Delivery List of authors.
Loïc Sentilhes, M.D., Ph.D., Marie V. Sénat, M.D.
April 29, 2021 N Engl J Med 2021; 384:1623-1634 DOI: 10.1056/NEJMoa2028788
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言








#预防性#
40
老药的新作用
53
#产后出血#
40
学习
58
顶刊就是顶刊,谢谢梅斯带来这么高水平的研究报道,我们科里同事经常看梅斯,分享梅斯上的信息
51
#学习#
66