Heart:Turner综合征女性主动脉扩张和生长情况
2022-06-22 MedSci原创 MedSci原创
在Turner综合征的女性患者中,升主动脉扩张较为常见,并与年龄、BAV和收缩压有关。
Turner综合征女性主动脉夹层的风险增加,这是一种与主动脉扩张相关的危及生命的事件。但是目前对于主动脉扩张随时间发展的了解仍然有限。
近日,心脏病领域权威杂志Heart上发表了一篇研究文章,该研究旨在描述主动脉扩张的患病率,以及寻找相关因素,并探究主动脉生长在Turner综合征患者中的情况。
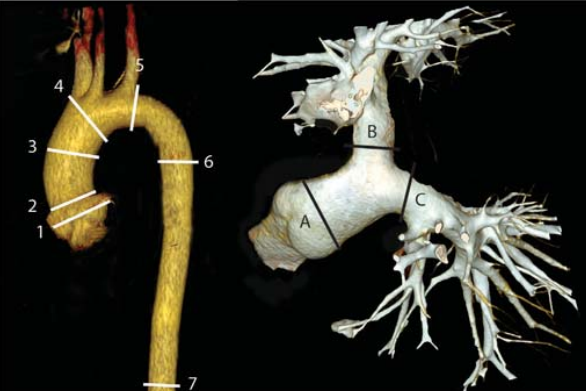
在这项前瞻性多中心队列研究中,研究人员纳入了2014年至2016年期间经基因证实为Turner综合征的连续就诊的成年女性,她们在基线和3年后接受心电图触发的多相CT血管造影检查。研究人员采用双斜重建法测量胸主动脉7节段的主动脉直径,并测量体表面积。升主动脉扩张定义为主动脉大小指数>20mm/m2。收集主动脉相关和心血管事件。统计分析包括线性和Logisitc回归和线性混合效应模型。
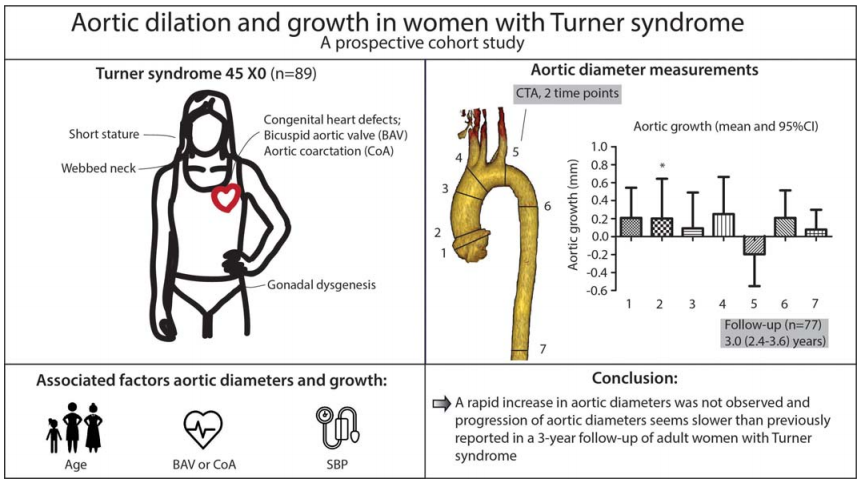
该研究的研究对象为89名女性,中位年龄为34岁(IQR为24-44)。基线时38.2%的患者伴有升主动脉扩张。年龄(OR为1.08(95%CI为1.03~1.13),p<0.001)、主动脉瓣二尖瓣(OR为7.09(95%CI为2.22~25.9),p=0.002)和收缩压(OR为1.06(95%CI为1.02~1.11),p=0.004)与升主动脉扩张独立相关。中位随访时间为3.0(2.4-3.6)年(n=77),仅在窦管交界处发现主动脉明显生长(0.20±1.92mm,p=0.021)。这些患者未发生主动脉夹层,一名患者接受了主动脉手术,一名女性死亡。
由此可见,在Turner综合征的女性患者中,升主动脉扩张较为常见,并与年龄、BAV和收缩压有关。
原始出处:
Frederike Meccanici.et al.Aortic dilation and growth in women with Turner syndrome.heart.2022.https://heart.bmj.com/content/early/2022/06/14/heartjnl-2022-320922
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#扩张#
37
#ART#
37
#主动脉#
49
#综合征#
41
#HEART#
44
#主动脉扩张#
33