AJRCCM:B细胞去除治疗系统性硬化症相关性肺动脉高压(SSC-PAH)的安全性和有效性
2021-10-16 刘少飞 MedSci原创
系统性硬化症 (SSc) 是一种罕见的全身性结缔组织疾病,其特征是皮肤和内脏器官的纤维化和萎缩;其多变的表现是由于自身免疫性微血管损伤和纤维化。当遗传、表观遗传和环境因素对免疫和血管系统产生负面影响时

系统性硬化症 (SSc) 是一种罕见的全身性结缔组织疾病,其特征是皮肤和内脏器官的纤维化和萎缩;其多变的表现是由于自身免疫性微血管损伤和纤维化。当遗传、表观遗传和环境因素对免疫和血管系统产生负面影响时,可能会发生疾病进展,导致纤维化重塑。 B 细胞功能异常可能导致致病性自身抗体、免疫失调和纤维化,因此,B 细胞免疫是该疾病某些表现的合理治疗靶点。肺动脉高压是 SSc 的一种严重并发症,临床前和临床研究表明 B 细胞和自身抗体在其发展中发挥了推定的作用。
SSc 患者的肺动脉高压有多种病因,包括进行性间质性肺病 (ILD)、肺静脉闭塞性疾病、慢性血栓栓塞性疾病、肺动脉高压 (PAH) 或这些因素的组合。有限的皮肤型 SSc 更常见于孤立的 PAH,也称为 SSc 相关的 PAH (SSc-PAH)。 SSc-PAH(当前研究的重点)在大约 10% 的 SSc 个体中发展。 SSc-PAH 患者更可能有严重的内在右心室功能障碍、高 BNP(B 型利钠因子)、低 DICO 和较差的存活率。 SSc-PAH 患者的肺表现出特征性的血管病理学;丛状病变比其他形式的 PAH 少见,血管病变显示血管周围淋巴细胞和内膜纤维化。 SSc-PAH 复杂的临床表现和独特的血管病理表明 I 组肺动脉高压疾病具有独特的生物学特性。人们越来越努力地了解自身免疫、炎症和 PAH 演变之间的关系。
由于 B 细胞免疫与 SSc 发病机制有关,因此在标准护理血管扩张剂治疗后,B 细胞耗竭是一种有吸引力的治疗候选药物。在其他 SSc 表现中,利妥昔单抗可减轻纤维化,因此它在减轻 SSc-PAH 的纤维增殖方面的益处是合理的。病例报告表明,利妥昔单抗可能对多种形式的 PAH 有治疗作用,最显着的是患有轻度 ILD 和重度 PAH 的难治性 SSc 患者。利妥昔单抗治疗 SSc-PAH 患者的发育性 B 细胞异常可暂时逆转。鉴于强有力的证据表明自身免疫性血管损伤和 SSc-PAH 患者的生存率低,谨慎处理 B 细胞耗竭的假定益处似乎是合理的。在这里,我们试图针对与 SSc 微血管损伤有关的适应性免疫臂。我们设计并实施了一项概念验证、多中心、双盲、安慰剂对照、随机临床试验,以评估利妥昔单抗对 5 年内诊断出的 SSc-PAH 患者的安全性、耐受性和潜在疗效。该试验侧重于无严重 ILD 的孤立组 I 肺动脉高压患者。我们假设使用利妥昔单抗去除 B 细胞会改善 SSc-PAH 患者的运动耐量。这些研究的一些结果之前已经以摘要的形式报道过。
研究目的:研究了 B 细胞耗竭治疗 SSc-PAH 的安全性和有效性。
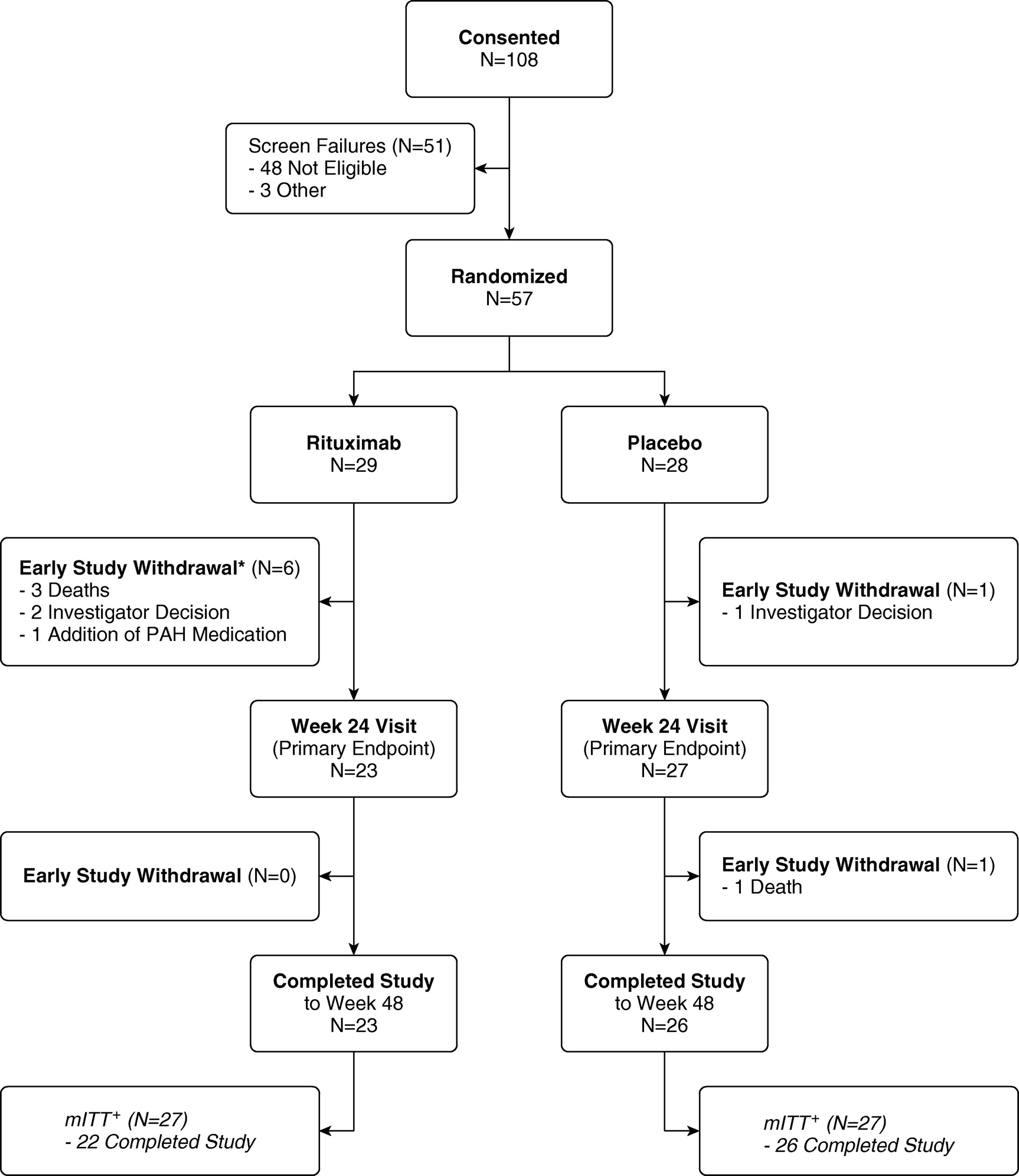
研究方法:在一项 NIH 赞助的、多中心、双盲、随机、安慰剂对照、概念验证试验中,57 名接受稳定剂量标准药物治疗的 SSc-PAH 患者接受两次 1,000 mg 利妥昔单抗或安慰剂输注间隔2周。主要结局指标是 24 周时 6 分钟步行距离 (6MWD) 的变化。次要终点包括安全性和侵入性血流动力学。我们应用机器学习方法来预测药物反应。
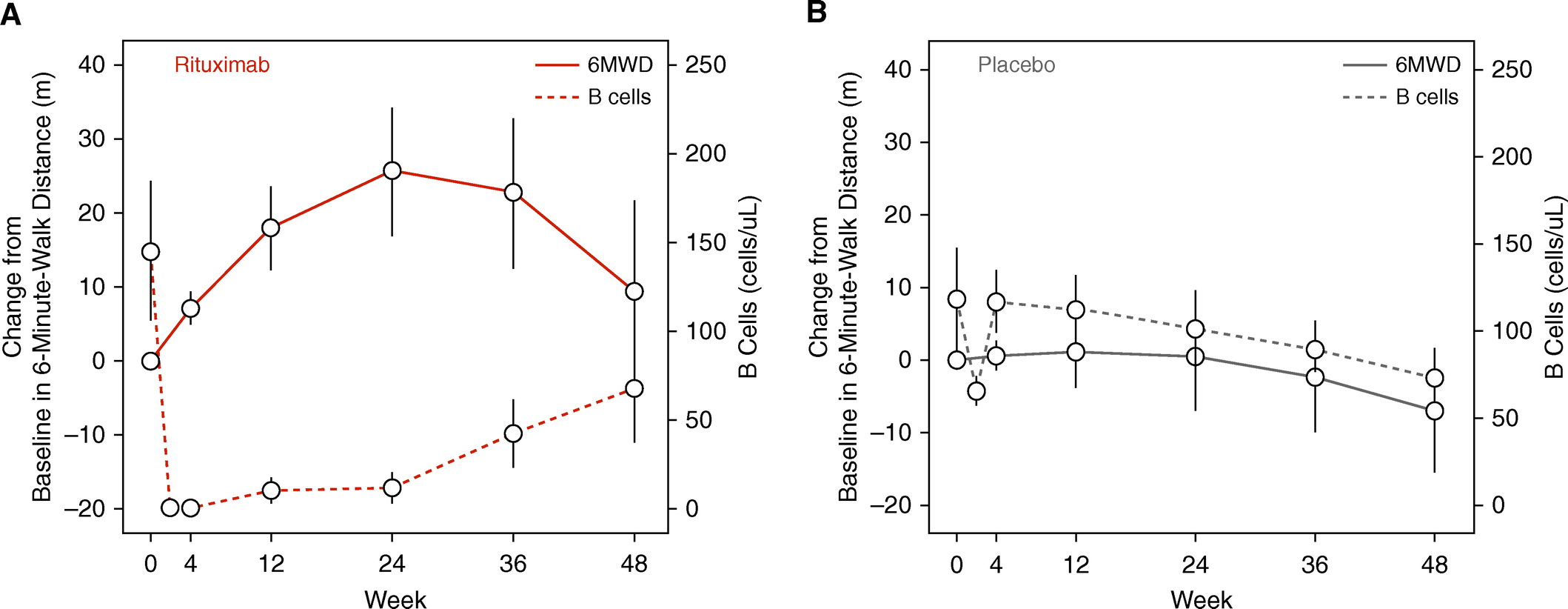
测量和主要结果:我们从 2010 年到 2018 年随机分配了 57 名受试者。在主要分析中,使用第 24 周的数据,24 周时 6MWD 的调整平均变化有利于治疗组,但没有达到统计学显着性(23.6 ± 11.1 m vs .0.5 ± 9.7 m;P = 0.12)。虽然是一项阴性研究,但当还考虑到第 48 周的数据时,利妥昔单抗在第 24 周的 6MWD 估计变化为 25.5 ± 8.8 m,安慰剂为 0.4 ± 7.4 m(P = 0.03)。利妥昔单抗治疗似乎安全且耐受性良好。低水平的 RF(类风湿因子)、IL-12 和 IL-17 作为利妥昔单抗反应的有利预测因子是敏感和特异的,如通过改善的 6MWD(曲线下的受体操作特征面积,0.88-0.95)测量的。
研究结论:B 细胞耗竭疗法是一种潜在有效且安全的 SSc-PAH 辅助治疗方法。未来对这些患者的研究可以确认已识别的生物标志物是否可以预测利妥昔单抗的反应性。
文章出处:
Zamanian RT, Badesch D, Chung L, Domsic RT, Medsger T, Pinckney A, Keyes-Elstein L, D'Aveta C, Spychala M, White RJ, Hassoun PM, Torres F, Sweatt AJ, Molitor JA, Khanna D, Maecker H, Welch B, Goldmuntz E, Nicolls MR. Safety and Efficacy of B-Cell Depletion with Rituximab for the Treatment of Systemic Sclerosis-associated Pulmonary Arterial Hypertension: A Multicenter, Double-Blind, Randomized, Placebo-controlled Trial. Am J Respir Crit Care Med. 2021 Jul 15;204(2):209-221. doi: 10.1164/rccm.202009-3481OC. PMID: 33651671.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#RCC#
43
#系统性#
34
#动脉高压#
32
#硬化症#
31
#安全性和有效性#
41
#相关性#
26
#B细胞#
41
#PAH#
30
#SSc#
36
#系统性硬化#
26