Nat. Genet:研究发现癌症干细胞标志蛋白
2013-02-07 Nat. Genet 中国科学报
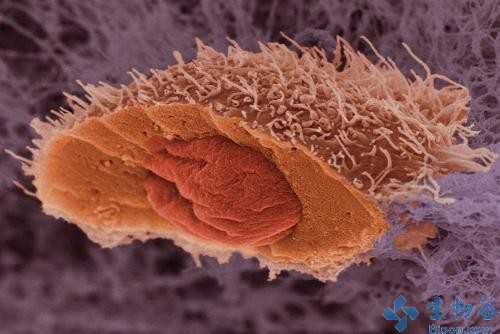
治疗癌症如果不把癌症干细胞彻底清除,癌症很容易复发和转移。日本京都大学的研究人员日前表示,他们找到了癌症干细胞含有的一种标志蛋白,有望对癌细胞做到“斩草除根”。 京都大学消化内科教授千叶勉领导的研究小组在研究中注意到消化道中的一种蛋白质Dclk1,他们分析了罹患大肠癌的实验鼠,发现含这种蛋白质的细胞会在较长一段时间内持续产生癌细胞。 该研究小组通过基因操作成功并有选择地清除了含Dclk1蛋白质
治疗癌症如果不把癌症干细胞彻底清除,癌症很容易复发和转移。日本京都大学的研究人员日前表示,他们找到了癌症干细胞含有的一种标志蛋白,有望对癌细胞做到“斩草除根”。
京都大学消化内科教授千叶勉领导的研究小组在研究中注意到消化道中的一种蛋白质Dclk1,他们分析了罹患大肠癌的实验鼠,发现含这种蛋白质的细胞会在较长一段时间内持续产生癌细胞。
该研究小组通过基因操作成功并有选择地清除了含Dclk1蛋白质的细胞,实验鼠体内的大肠癌组织面积缩小了80%以上,有些甚至完全消失,而且未发现副作用。
治疗癌症如果不把癌症干细胞彻底清除,则癌症很容易复发和转移,因此必须找到癌症干细胞,对其“斩草除根”。
而此前人们陆续发现的癌症干细胞所含的一些标志物质同时也存在于正常干细胞内,如果以这些物质为目标清除癌症干细胞的话,会误伤到正常干细胞,导致副作用的出现。

doi:10.1038/ng.2481
PMC:
PMID:
Dclk1 distinguishes between tumor and normal stem cells in the intestine
Yuki Nakanishi, Hiroshi Seno, Ayumi Fukuoka, Taro Ueo, Yuichi Yamaga, Takahisa Maruno,Naoko Nakanishi, Keitaro Kanda, Hideyuki Komekado, Mayumi Kawada, Akihiro Isomura,Kenji Kawada, Yoshiharu Sakai, Motoko Yanagita, Ryoichiro Kageyama, Yoshiya Kawaguchi, Makoto M Taketo, Shin Yonehara & Tsutomu Chiba
There is great interest in tumor stem cells (TSCs) as potential therapeutic targets; however, cancer therapies targeting TSCs are limited. A drawback is that TSC markers are often shared by normal stem cells (NSCs)1, 2, 3, 4; thus, therapies that target these markers may cause severe injury to normal tissues. To identify a potential TSC-specific marker, we focused on doublecortin-like kinase 1 (Dclk1). Dclk1 was reported as a candidate NSC marker in the gut5, 6, but recent reports have implicated it as a marker of differentiated cells (for example, Tuft cells)7, 8. Using lineage-tracing experiments, we show here that Dclk1 does not mark NSCs in the intestine but instead marks TSCs that continuously produce tumor progeny in the polyps of ApcMin/+ mice. Specific ablation of Dclk1-positive TSCs resulted in a marked regression of polyps without apparent damage to the normal intestine. Our data suggest the potential for developing a therapy for colorectal cancer based on targeting Dclk1-positive TSCs.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言












#Nat#
29
#Genet#
35
#研究发现#
29
#Gene#
35
#NET#
26
#癌症干细胞#
30