JAMA:射频神经切断术用于慢性腰痛的治疗
2017-07-05 zhangfan MedSci原创
对于关节突疼痛、骶髂关节痛患者以及关节突、骶髂关节或椎间盘痛的患者,射频神经切断术联合运动训练相比于单独的运动训练不能显著改善慢性腰痛患者症状,该研究结果不能支持射频神经切断术用于慢性腰痛的治疗
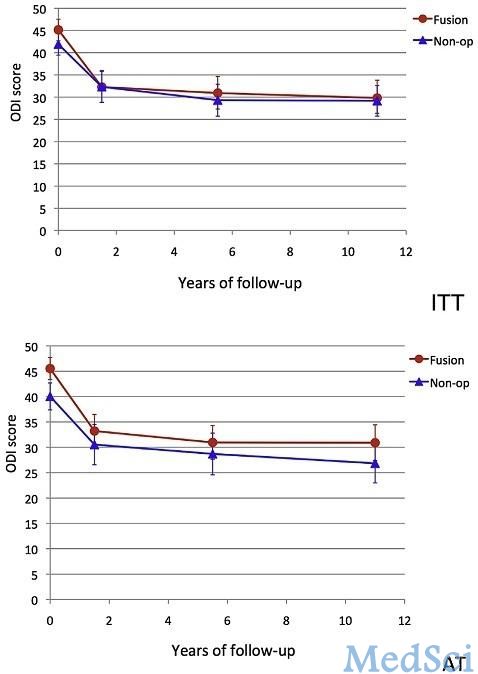
射频神经切断术是治疗慢性腰痛的常用方法,但高质量的疗效证据较少。近日研究人员考察了射频神经切断术联合运动训练用于慢性腰痛患者的效果。研究在荷兰的16个多学科疼痛治疗中心开展,对慢性腰痛患者进行微创介入治疗的疗效观察,研究从2013年1月至2014年10月。参与研究的慢性腰痛患者包括:251人关节突疼痛患者,228名骶髂关节痛患者以及202名关节突、骶髂关节或椎间盘联合痛患者,所有患者对保守治疗反应不显著。参与者先接受3个月的标准运动锻炼和心理辅导。干预组患者接受射频神经切断术,干预通常进行1次,试验中最大干预次数不超过3次。主要的终点是3个月后的疼痛强度评价(0-10,0代表无痛,分数高疼痛加重),预先设定的最小临床重要差异为2分或以上共681人参与研究,患者平均年龄52.2岁,其中61.8%为女性,平均基线疼痛强度为7.1。88%的患者完成3个月随访,77%的患者完成12个月的随访。干预组与对照组3个月的疼痛差异如下:关节突疼痛,-0.18 (95% CI,-0.76-0.40);骶髂关节痛-0.71 (95% CI,-1.35- -0.06)、关节突、骶髂关节或椎间盘痛-0.99
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言










#切断术#
48
学习了,临床有待进一步研究
53
学习了新知识,临床应用看来还有待研究。
65
#慢性腰痛#
42
希望早点用于临床那位,拜托你看清楚结论。
55
学习了谢谢分享
56
希望广泛应用于临床
63
学习了新知识
32
谢谢分享,学习了
32
学习了受益匪浅。
39