近年来我国炎症性肠病(IBD)的发病率显著升高,其诊治已经成为消化科面对的主要挑战之一。IBD具有慢性发展、反复发作的临床特点,腹泻、腹痛、便血等症状给患者造成了极大困扰,严重时还可能导致消化道大出血、穿孔、肠梗阻、癌变等并发症,对生活质量产生较大的负面影响[1]。早期使用生物制剂积极治疗可以有效控制肠道炎症,减少并发症的产生,降低手术率,获得更好的预后,甚至在一定程度上改变疾病的自然病程。如何选择适合我国IBD患者的生物制剂?通过分析生物制剂治疗中国IBD患者的真实世界数据,可真正为广大消化科医生的临床决策指明方向。 现有生物制剂方案表现如何? 生物制剂已成为传统治疗疗效不佳或不耐受的中重度IBD患者的一线治疗方案[2]。目前常用的生物制剂包括抗肿瘤坏死因子(TNF-α)药物、抗整合素类药物和白介素(IL)抑制剂类药物等。但对抗TNF-α治疗无应答(PNR)或随着时间延长失应答(LOR)的患者比例分别高达40%和约24%-46%。EXPLORE研究中国亚组结果显示,我国>50%IBD患者对抗TNF-α一线治疗应答不佳[3]。维得利珠单抗(VDZ)是一种肠道选择性生物制剂,通过特异性拮抗α4β7整合素,阻止T淋巴细胞向肠道迁移,从而减少肠道炎症反应,具有精准靶向性。既往国外的多项真实世界研究证实维得利珠单抗的临床有效性和安全性,但其应用于对中国患者的疗效和安全性数据仍有待累积。近期发布的一篇维得利珠单抗治疗中国IBD患者的真实世界数据为我们提供了宝贵经验,具有重要临床实践参考价值。一起来看看其表现如何? 最新中国证据,验证维得利珠单抗治疗IBD患者的真实世界疗效和安全性良好 近日,已正式发表于《临床与病理杂志》的一项单中心回顾性研究,明确维得利珠单抗在IBD患者应用的短期疗效与安全性,对于指导我国IBD临床实践提供了重要的参考和借鉴。来自中山大学附属第六医院消化科的郅敏教授作为通讯作者,姚嘉茵教授为论文的第一作者[4]。 研究者回顾性收集2020年11月1日至2021年10月31日在中山大学附属第六医院IBD诊疗中心使用维得利珠单抗治疗的52例IBD患者(39例CD患者,13例UC患者),均使用维得利珠单抗标准治疗。使用克罗恩病疾病活动指数评分(CDAI)评估CD疾病严重程度,CDAI评分<150定义为临床缓解,CDAI评分下降≥70为临床应答。使用克罗恩病简化内镜评分(SES-CD)评估CD的内镜严重程度,SES-CD评分≤2为内镜下缓解,SES-CD评分下降≥50%为内镜应答。使用改良Mayo评分评估UC患者的疾病活动度,改良Mayo评分≤2分且无单个分项评分>1定义为临床缓解。评分相对于基线值的降幅≥30%以及≥3分,而且便血的分项评分降幅≥1分或该分项评分为0或1分定义为临床应答。使用Mayo内镜评分评估UC内镜病变程度,Mayo内镜评分0或1分定义为内镜缓解。Mayo内镜评分较基线下降≥1分定义为内镜应答。同时记录VDZ治疗的不良反应。每次入院输注VDZ时均予临床活动度评分(CDAI或改良Mayo),记录营养指标[体重指数(BMI)、白蛋白(Alb)、血红蛋白(Gb)]及炎症指标[血沉(ESR)、C反应蛋白(CRP)],且在22周(第5次VDZ时)复查内镜,评估内镜下改变(SES-CD或内镜Mayo评分)。 治疗22周后,CD患者的疾病活动度及内镜改变如何? 39例CD患者的平均年龄为30.3±9.8岁,男性占66.7%,平均病程80.1±57.7个月。治疗22周后,患者的CRP(12.8±10.0 vs 10.5±4.7,P=0.03)及ESR (18.1±12.0 vs 13.0±3.8,P<0.01)较基线值显著下降,HGb (129.6±20.8 vs 122.3±23.4,P<0.01)及BMI (20.2±3.3 vs 19.5±3.3,P<0.01)较基线值显著升高。CD患者的临床缓解率71.4%,临床应答率87.2%,共17例患者有前后SES-CD评分对比,分析得出其内镜缓解率为29.4%,内镜应答率为76.5%。 治疗22周后,UC患者的疾病活动度及内镜改变如何? 13例UC患者的平均年龄为40.6±18.1岁,男性占46.2%,平均病程101.8±105.2个月。维得利珠单抗治疗22周后,患者的ESR(12.2±12.3 vs 28.8±26.4,P<0.05)较基线值显著下降,HGb(118.2±16.5 vs 107.4±19.1,P<0.05)较基线值显著升高。UC患者的临床缓解率为53.9%,临床应答率为76.9%,内镜缓解率与内镜应答率均为57.1%。 安全性分析 在56例IBD患者中,1例患者出现过敏性皮疹,经过抗过敏治疗后皮疹消退,维得利珠单抗治疗的不良反应率仅为0.02%(1/56)。 图1 维得利珠单抗治疗22周时, CD与UC患者的临床及内镜改善情况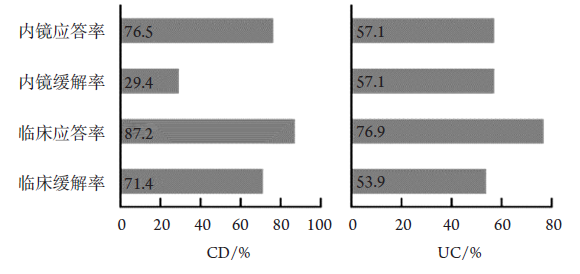
综上,本研究表明,维得利珠单抗短期应用有效诱导及维持IBD患者疾病缓解,并且促进黏膜愈合,不良反应率低,安全性高。开展本研究的中山大学附属第六医院IBD中心是国内较大的IBD诊疗中心之一,诊疗过程规范,数据记录完整,患者随访规律,因此本研究数据可信度高,更是从黏膜愈合的高度评价维得利珠单抗对内镜缓解的作用。
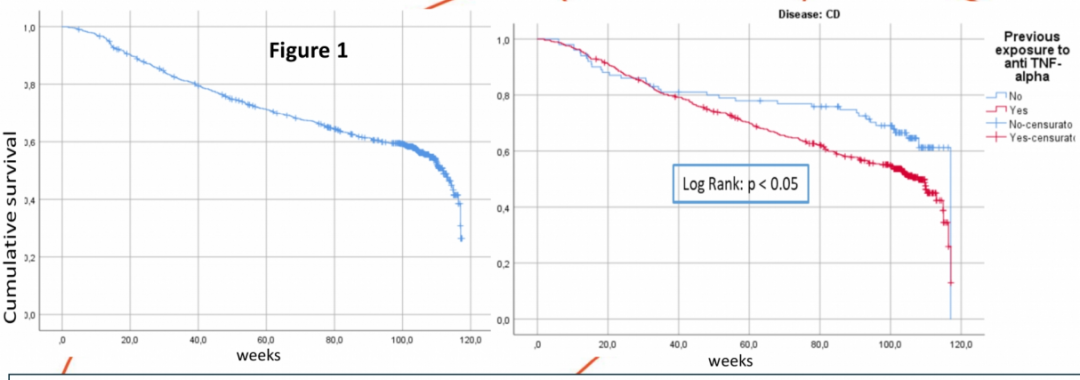
和本研究结果一致,国外已累积了丰富的维得利珠单抗真实世界数据。2021 DDW发布的意大利真实世界LIVE研究是一项大规模IBD患者队列研究,旨在评估真实世界中维得利珠单抗的长期疗效与安全性[5]。研究纳入意大利47个IBD中心的1111例患者(CD患者564例,UC患者547例),256例(23%)为生物制剂初治患者。结果显示,维得利珠单抗持续治疗达12个月和24个月的比例分别为73.3%和67.3%,且CD患者中生物制剂初治组的持续治疗时间显著长于生物制剂经治组。总体安全性良好。
图2 维得利珠单抗治疗2年的累积生存率
总结
随着IBD逐渐成为消化科的常见病之一,在众多生物制剂中,如何选择合适的治疗方案是关键。但我国超过一半IBD对抗TNF-α一线治疗应答不佳。中山六院发表的这项最新真实世界数据,验证了维得利珠单抗治疗我国IBD患者的短期疗效良好,可有效促进IBD患者黏膜愈合,且安全性良好。未来需要多中心大样本的数据进一步评估其短期与长期疗效,为更多IBD患者真正能够在临床中获益积累经验。
参考文献:
1. 周青杨, 钱家鸣. 新型肠道选择性生物制剂治疗炎症性肠病的研究进展[J]. 中华消化杂志. 2020; 40(2): 141-144.
2. 中华医学会消化病学分会炎症性肠病学组. 中华消化杂志, 2021,41(06):366-378.
3. Li J, et al. BMC Gastroenterol. 2022 Feb 4;22(1):44. PMID: 35120446.
4. 姚嘉茵, 郅敏, 等. 维得利珠单抗治疗炎症性肠病的短期疗效与安全性:单中心真实世界研究[J]. 临床与病理杂志, 2022, 42(8): 1841-1846. doi: 10.3978/j.issn.2095-6959.2022.08.009
5. Daniela Pugliese, et al. ITALIAN REAL-LIFE STUDY EVALUATING THE LONG-TERM EFFECTIVENESS OF VEDOLIZUMAB FOR THE TREATMENT OF INFLAMMATORY BOWEL DISEASE. DDW 2021. Abstract Su459.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言














#最新#
42
#选择性#
49
#生物制剂#
73
#IBD#
59
#真实世界#
53