闭合性胸锁关节脱位合并金黄色葡萄球菌感染1例
2020-04-20 向飞帆 周举 梁杰 中国骨伤
患者,男,60岁,重物压砸致上胸部疼痛2周,呼吸困难3d入院。患者2周前搬抬重物时不慎被砸中上胸部,当即出现上胸部疼痛,右肩活动时疼痛加重。在当地医院就诊予以对症治疗(具体过程不详),患者症状无明显缓
临床资料
患者,男,60岁,重物压砸致上胸部疼痛2周,呼吸困难3d入院。患者2周前搬抬重物时不慎被砸中上胸部,当即出现上胸部疼痛,右肩活动时疼痛加重。在当地医院就诊予以对症治疗(具体过程不详),患者症状无明显缓解。3d前出现呼吸困难,于我院急诊科行CT检查示右侧包裹性胸腔积液,右胸锁关节脱位。以右胸锁关节脱位,右侧包裹性胸腔积液收入院。
入院查体:右胸锁关节隆起,较健侧突出,明显红肿,皮温稍高,无明显包块,未扪及波动感。右胸锁关节周围压痛,右肩关节活动时疼痛加重(图1a,1b)。血常规示WBC10.02×109/L,血沉150mm/h。入院后予以吸氧、止痛、预防感染等对症治疗。病情稳定后完善CT三维重建提示右胸锁关节脱位(图1c,1d)。术前检查血常规示:WBC6.07×109/L,血沉120mm/h。在全麻下行清创+胸锁关节脱位复位克氏针固定+韧带修复术。患者取沙滩椅位,术前见右胸锁关节处约2cm×3cm的隆起,皮温稍高,以隆起处为中心,沿锁骨走形取长约5cm的切口,切开皮肤,分离皮下组织,探查见右胸锁关节周围较多脓性分泌物,右胸锁关节中心型脱位,胸锁前韧带断裂。彻底清创后,复位胸锁关节,克氏针固定,2-0肌腱线修复胸锁前韧带(图1e,1f)。术中取分泌物进行病理检查及细菌培养,病理检查结果示炎性组织增生,细菌培养为金黄色葡萄球菌,结核芯片检查未提示异常(图1g)。
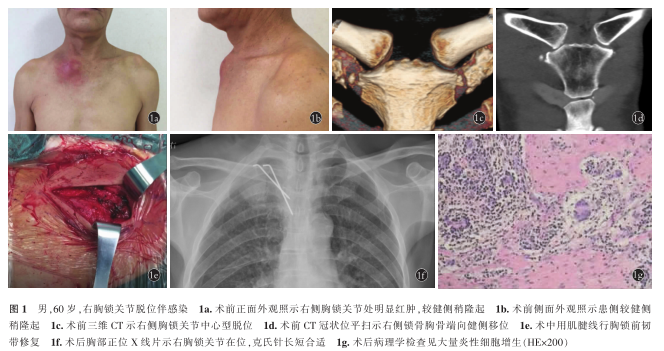
术后体温正常,伤口未见明显红肿、无渗血渗液,患者一般情况良好,未见明显感染迹象,继续予以抗感染等对症治疗,悬吊患肢。术后1个月复查血常规、CRP、血沉未见异常,伤口乙级愈合。
讨论
(1)闭合性脱位伴感染原因。本例患者为闭合性脱位,胸前区皮肤无擦伤、裂伤等情况。患者因包裹性胸腔积液伴呼吸困难入院。胸腔积液后,肺部排痰能力下降,容易并发肺部感染;同时由于创伤可能导致短暂的免疫抑制。因此,肺部等邻近部位感染可能导致闭合性胸锁关节脱位并发感染。胸锁关节属于上肢微动关节,发生胸锁关节感染非常罕见。一般发生在具有感染高危风险的患者身上,通常是单侧的。本例患者因外伤致创伤性湿肺,具有感染高危风险。McAninch等报道了1例没有明显危险因素的患者,最初表现为左胸、左颈肩疼痛,抗生素治疗可能的肺炎,症状复发,随着初始症状发作后反复发烧,最后放射学诊断左侧胸锁关节感染。目前闭合性骨折合并感染的报道较多,但闭合性脱位并发感染的情况相对较少。
(2)闭合性脱位伴感染治疗方式。本例患者术前血常规提示白细胞总数和中性粒细胞比例均未明显升高,但血沉升高。术前未引起重视,术中探查发现感染,决定行清创、克氏针固定、韧带修复。在无明显危险因素的情况下,闭合性骨折脱位合并感染的诊断相对困难。血沉在闭合性骨折脱位合并感染的诊断中有一定的帮助。这也提示临床医师在以后的诊疗工作中需要更加重视血沉、CRP、PCT等感染指标的作用。本例患者术中探查发现胸锁关节中心型脱位,胸锁前韧带断裂,由于存在感染,本例患者采取了清创+复位克氏针固定+韧带修复术,有效地控制了感染,同时行复位脱位的胸锁关节。胸锁关节脱位分型可分为前脱位、后脱位和中心脱位,其中以前脱位较为常见。本例为中心脱位,其发生机制主要为直接暴力所致。胸锁关节脱位的固定方式较多,刘攀等采用锁骨钩钢板固定胸锁关节脱位,锁骨钩钢板能在复位固定胸锁关节的同时保留胸锁关节微动功能,且不损伤胸锁关节软骨面,手术安全性高,固定效果好,患者术后可进行早期康复锻炼。钢板内固定的稳定性应该比克氏针高,但由于感染的原因,放置钢板内固定风险太高,因此,本例患者优先控制感染,在控制感染的同时行克氏针固定,取得了较为理想的效果。
通过对本例患者的诊治,提示在临床诊疗过程中无论开放还是闭合骨折脱位,都需要警惕感染的可能,密切关注CRP等感染指标,有助于感染的预防和治疗。
原始出处:
[1]向飞帆,周举,梁杰,叶俊武,阳运康.闭合性胸锁关节脱位合并金黄色葡萄球菌感染1例[J].中国骨伤,2020,33(03):281-282.
本网站所有内容来源注明为“梅斯医学”或“MedSci原创”的文字、图片和音视频资料,版权均属于梅斯医学所有。非经授权,任何媒体、网站或个人不得转载,授权转载时须注明来源为“梅斯医学”。其它来源的文章系转载文章,或“梅斯号”自媒体发布的文章,仅系出于传递更多信息之目的,本站仅负责审核内容合规,其内容不代表本站立场,本站不负责内容的准确性和版权。如果存在侵权、或不希望被转载的媒体或个人可与我们联系,我们将立即进行删除处理。
在此留言













#闭合性胸锁关节脱位#
25
#胸锁关节脱位#
28
#关节脱位#
34
#金黄色葡萄球菌#
34
#脱位#
31
#葡萄球菌#
28
辛苦分享
91